Paediatric asthma: update on the stepwise management approach

The updates to both national (Australian Asthma Handbook) and international (Global INitiative for Asthma, GINA) guidelines over recent years have included major updates to evidence and advice on managing asthma in infants and children. Enhanced adherence to these guidelines is crucial for efforts to address the ongoing concern about preventable asthma deaths in Australia.
Note
This is an online update of the original version of this article that was published in the September 2020 issue of Respiratory Medicine Today. This update was prepared for World Asthma Day 2024.
- The stepwise approach to management of childhood asthma differs by age group (0 to 12 months, 1 to 5 years, 6 to 11 years and 12 years and over).
- Before any stepwise increase in asthma preventer treatment, clinicians should reconsider the diagnosis of asthma, check the parents’ and child’s understanding of asthma management and treatment adherence, and minimise exposure to triggers and environmental tobacco smoke.
- Asthma should be considered as a chronic remitting and relapsing condition, with any hospital presentation representing evidence of inadequate disease control.
- Asthma exacerbations should be considered as a red flag and prompt review of current management.
- Children should be referred for specialist paediatric assessment if they have:
– continued poor symptom control or persistently abnormal spirometry: expiratory airflow limitation or airway hyper-reactivity, despite prescription of an appropriate asthma preventer
– more than two courses of systemic corticosteroids per year or more than one hospital presentation per year
– limitations on school attendance or participation in activities
– any life-threatening episode of asthma.
In Australia, the prevalence of asthma in children aged 0 to 14 years approaches 10%, with higher rates among First nations (i.e. Aboriginal and Torres Strait Islander) people and those living in lower socioeconomic areas.1 Asthma is the fourth most common paediatric emergency presentation and the sixth most common reason for referral to a paediatrician.2,3 The National Asthma Council Australia publishes treatment guidelines in the Australian Asthma Handbook (AAH), based on evidence, where available, and on expert consensus opinion. Recent updates released over the past five years (versions 2.0-2.2) included major updates to evidence and advice on managing asthma in infants and children.Changes affecting the use of preventer as reliever treatment for adolescents included in these updates are also discussed here.4 These changes reflect similar changes that have occurred in the major internal guidelines such as the Global INitiative for Asthma (GINA) guidelines over the same time period.5
Despite widespread availability of national and international asthma management guidelines, clinician adherence to guidelines remains inadequate and inferior to the reported adherence for many other chronic conditions.6 Most clinicians asked about the frequency of rescue inhaler use, but the impact of asthma on normal daily activities and frequency of nocturnal symptoms were less well monitored.7 Provision of a written asthma plan, observation of inhaler technique, use of preventer medication and the approach to ‘difficult-to-control’ asthma have been identified as areas for improvement for primary care clinicians.7,8 Families identify GPs among their most trusted resources for asthma management, reinforcing their important role.9
This article summarises the current stepwise approach to asthma management in children recommended in AAH version 2.2 and outlines age-specific aspects that GPs should consider. It updates the review of age-specific management of asthma in children, published five years ago in the 2019 issue of Medicine Today, which was based on previous AAH versions.10
We also discuss the ongoing concern that asthma deaths, which should be viewed as preventable, continue to occur far too often and that poor asthma control or recent hospitalisation should be recognised as significant ‘red flags’ (i.e. risk factors) for poor outcomes.11-14 Finally, we describe key aspects of the management of difficult-to-treat asthma at tertiary paediatric institutions to provide context for the medications and approaches GPs may encounter as they share management in primary care.
Treatment guidelines by age
The stepwise treatment approach by age in the AAH categorises children into those aged 0 to 12 months, 1 to 5 years, 6 to 11 years and adolescents, with the last age category classed together with adults. Within these age groups, pertinent aspects of acute management of wheeze and ongoing maintenance asthma preventer treatment are discussed below. Several statements, although introduced within a particular ordinal age group, have broad relevance across all age groups.
Early childhood wheeze is a highly heterogeneous condition, with several wheeze phenotypes described by important longitudinal cohort studies.15 These wheeze phenotypes are identifiable by the early temporal pattern of wheeze and whether symptoms persist into school age.
In the past, two different approaches to classifying early childhood wheeze phenotypes, occurring in the first six years of life, have been proposed:
- a symptom-based classification – ‘episodic viral wheeze’ in which wheeze occurs in discrete time periods predominantly associated with upper respiratory tract infection with a lack of symptoms between episodes, and ‘multiple-trigger wheeze’ where wheezing occurs between these episodes and may be triggered by a range of triggers (e.g. change in weather, activity, emotion)
- A temporal-based classification – ‘transient wheeze’ (onset and resolution of symptoms within the first three years of life), ‘persistent wheeze’ (onset before three years and continuation of symptoms beyond six years of age) and ‘late-onset wheeze’ (symptom onset after the age of three years).
However, both approaches have limitations with neither performing well when applied prospectively and there is ongoing work within large birth cohort studies to find improved approaches for clinical use.17,18 A recent example of this work is the CHILDhood Asthma Risk Tool (CHART) which was developed, and subsequently validated, for its ability to identify children with asthma or persistent symptoms at five years of age based on identified factors associated with asthma at 3 years of age (timing and number of wheeze or cough episodes, use of asthma medications, and emergency department visits or hospitalizations for asthma or wheeze).19 These tools have yet to be incorporated into clinical care.
Children 0 to 12 months
Infants aged 0 to 12 months are considered separately from older children in the 2020 AAH. This change acknowledges the differences in wheeze mechanisms between infants and preschool-aged children and seeks to avoid potential harm due to inappropriate treatment.
Management of acute wheeze in infants
Bronchiolitis is an important cause of acute wheezing, and later wheezing episodes are more likely in children who have been hospitalised with bronchiolitis. Reassuringly, most of these children do not require subsequent hospitalisation. In a longitudinal cohort study of more than 20,000 infants in the UK, 80% of those with relatively severe bronchiolitis (i.e. requiring hospitalisation in the first year of life) did not have further wheezing episodes within the study period, which followed up children to the age of 8 years.20 This year has seen the introduction and roll out of Nirsevimab an injectable long-acting monoclonal antibody that protects against respiratory syncytial virus (RSV) infection, the most common cause of hospitalisation for bronchiolitis in infants. In clinical trials nirsevimab reduced the incidence of hospitalisation for RSV associated lower respiratory tract infection by 76 to 78% among preterm-term infants entering their first RSV season compared to placebo.21 It has been estimated that avoiding RSV infection during infancy may reduce asthma diagnosis rates at age five years by approximately 15%.22
Recent evidence-based Australasian guidelines on bronchiolitis recommend against routinely trialling short-acting bronchodilator or systemic corticosteroid therapy for infants aged 12 months and younger with bronchiolitis.23 In this group, the predominant aetiology of wheeze is not airway hyperresponsiveness, but relates to small airway calibre, further narrowed by oedema and increased mucus secretion, for which beta2 agonists are ineffective.24 Furthermore, there is good evidence that beta2 agonists are of no benefit (for hospitalisation rate or length of stay) and in fact led to increased adverse events (tachycardia, hypertension, tremor and decreased oxygen saturation) for infants with bronchiolitis compared with placebo.25,26
The findings of a Cochrane review were based on large cohort studies; however, there is likely a small subset of infants who respond to beta2 agonists. The current recommendation from the National Asthma Council Australia is to consult a paediatrician before a therapeutic trial of a bronchodilator or corticosteroid (either inhaled or systemic).4 Identifying which infants should trial bronchodilators remains challenging, and for most infants’ supportive care (respiratory support and adequate hydration) is all that is required. However, in older infants and those with a history of atopy and a strong family history of asthma, a trial of beta2 agonists may be considered. Important considerations when trialling beta2 agonists are discussed in the older age groups. There is no role for routine corticosteroid therapy in infants with bronchiolitis nor in the subset of infants with a positive response to beta2 agonists.
Asthma preventer therapy in infants
Transient early wheeze is the most common wheeze phenotype in infants. It is generally not distressing for the infant, who thrives despite these symptoms. Cough and difficulty breathing are uncommon, and wheeze may be more prominent with viral illnesses. It is associated with lower initial lung function (which later improves) and is believed to be due to smaller calibre of airways. Therefore, this wheeze does not respond to bronchodilators nor to any other current asthma preventer medication. A three-year randomised placebo-controlled trial treated infants for two weeks following an episode of wheeze of at least three days’ duration. The study reported intermittent ICS had no effect on progression from episodic to persistent wheezing and no short-term benefit during these episodes of wheeze.27
Infants at increased risk of wheeze include:
- those born preterm (especially those with bronchopulmonary dysplasia)
- those with antenatal or environmental exposure to tobacco smoke
- those with previous bronchiolitis caused by respiratory syncytial virus (RSV) or recurrent rhinovirus infections.28
In these infants, viral infections continue to be the most common cause of exacerbations, but other triggers such as environmental tobacco smoke, aeroallergens and air pollution should be considered, and exposure minimised.29
Although the AAH does not give specific recommendations for infants with recurrent or persistent wheeze, insight can be gained from other sources.28 In a recent review, close follow up of infants with recurrent wheeze is recommended, and a trial of inhaled corticosteroid (ICS) with short-acting beta agonist (SABA) therapy as needed may be considered, with a re-evaluation of symptoms after a few weeks. If a good clinical response is observed, a dose reduction or cessation after a few months should be considered. If symptoms recur, continued treatment is indicated.28
Children aged 1 to 5 years
The AAH moved away from the pattern of symptoms (e.g. infrequent intermittent, frequent intermittent or persistent) to consider clinical severity outcomes to guide preventer management.4 Specific categories are:
- mild (salbutamol as needed at home)
- moderate-severe (requiring systemic corticosteroids and/or emergency department presentation)
- life-threatening (requiring hospitalisation or intensive care).
The recommended preventer medicines in this age group are ICS and montelukast (in children aged 2 years and above).
Wheeze is common in the preschool age group, with nearly one third of preschool-aged children having intermittent wheezing.30 Despite the high morbidity of early childhood wheeze, it is estimated that only 30% of toddlers with recurrent wheeze progress to asthma at age 6 years, and fewer still continue to have wheeze as adults.15
Management of acute wheeze in children 1 to 5 years
Salbutamol can be used on an ‘as-needed’ basis to relieve symptoms during wheezing episodes if a therapeutic trial shows it is beneficial. A child with wheeze who is eating well and playing, without signs of a prolonged expiratory phase or increased respiratory effort, may not require any treatment. When a trial of a bronchodilator is appropriate, the markers of clinical improvement should be considered a priori.
The most useful markers of a response include improvements in oxygen saturation, heart rate and respiratory rate, combined with subjective examination findings such as the child’s level of interaction, ability to speak or vocalise without limitation, use of accessory muscles, pronounced expiratory phase and changes in air entry or wheeze throughout the lung fields. Repeated clinical assessment is essential, and the response, or lack thereof, should be well documented in the clinical record and may indicate an alternative diagnosis.31,32
In the 1 to 5-year age group, viral-induced wheeze does not respond to systemic corticosteroids in the same way as observed in older age groups. Two randomised placebo-controlled trials of oral cortico-steroids (OCS) to treat viral-induced wheeze are worth mentioning. A 2009 UK study found no difference in hospital admission rates, whereas a 2018 Perth study reported a relatively modest effect on the duration of hospital stay (less than three hours difference vs placebo).33,34 These differing results may reflect potential inclusion of infants with bronchiolitis in the first study.35 In the acute inpatient setting, OCS use should be reserved for those with a clinical response to bronchodilators and a high clinical suspicion of allergic asthma.36,37
Asthma preventer therapy in children aged 1 to 5 years
Episodic viral-induced wheeze is the most common wheeze presentation, with children having no symptoms between discrete episodes. Multiple-trigger wheeze describes wheeze with additional triggers, such as exercise, allergens, cold air and smoke.29 Multiple-trigger wheeze is more likely to persist into older age groups and is associated with greater impairment of lung function and atopy (asthma, hayfever, eczema or allergies) than viral-induced wheeze.38 As mentioned earlier, application of this ERS categorisation in clinical practice can be challenging, as the features may change over time for individual children in the preschool age range.39
As in other age groups, environmental tobacco smoke exposure must be acknowledged to families as an important trigger, and support offered for smoking cessation. A meta-analysis reported the effects of environmental tobacco smoke exposure on asthma morbidity in children aged 0 to 18 years; environmental tobacco smoke was associated with worsening lung function, increased wheeze symptoms and nearly double the rates of hospitalisation for acute asthma compared with children not exposed.40
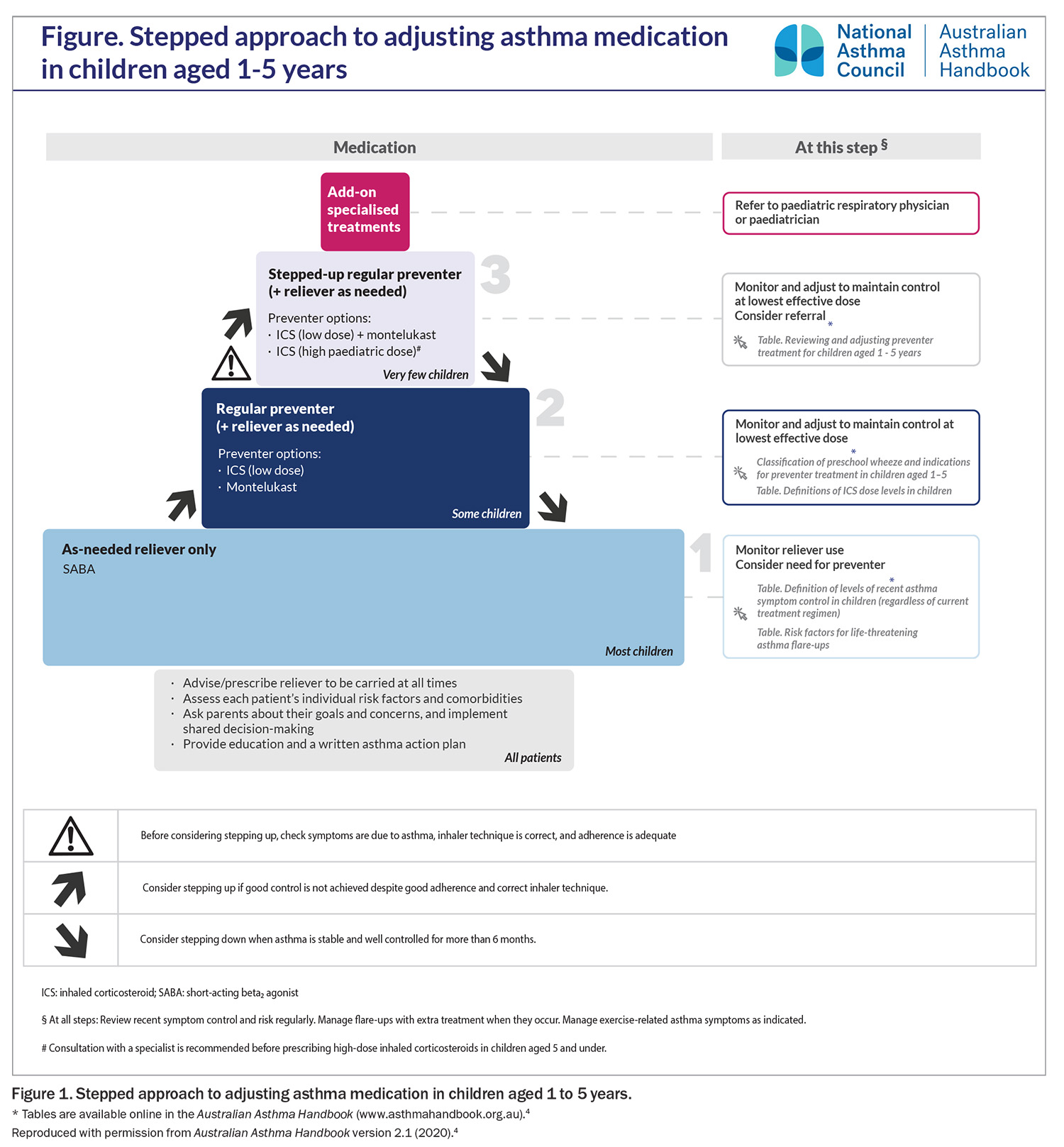
The stepwise approach to maintenance asthma preventer treatments for children aged 1 to 5 years is shown in Figure 1. A trial of preventer therapy is indicated in children with:
- recurrent episodic symptoms at least once per week or less often if associated with more severe symptoms (OCS treatment or hospital presentation)
- severe symptoms (OCS treatment or hospital presentation)
- a demonstrated response to bronchodilator therapy, and
- clinical features associated with increased risk of asthma.4
Inhaled corticosteroid is the preferred first line preventer treatment for those with frequent symptoms or infrequent but severe exacerbations. A leukotriene receptor antagonist (LTRA) may be considered if the child is unable to use a spacer and MDI or parents decline ICS or are significantly concerned of the side effects (likely to have poor adherence).41 In preschool-aged children with persistent wheeze, both ICS and LTRA have been shown to reduce SABA and OCS use, as well as the frequency of asthma symptoms.42 The adverse effects of ICS and LTRA are described in the next section but are also applicable to this age group. LABA are not licensed for this age group, and the effects of LABA plus ICS have not been studied systematically in children younger than 4 years.
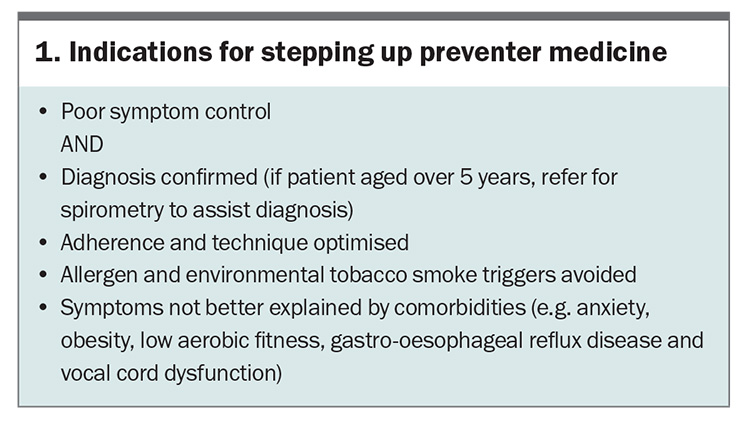
The indications for stepping up preventer therapy are listed in Box 1. Before any increase in preventer therapy, clinicians must:
- confirm symptoms due to asthma rather than concurrent or alternate diagnosis
- assess patient and family understanding of asthma management and the role of reliever and preventer medicines
- assess adherence to current preventer medicine
- assess spacer technique
- determine whether comorbid obesity, gastro-oesophageal reflux, anxiety or inducible laryngeal obstruction better account for symptoms
- minimise exposure to asthma triggers and environmental tobacco smoke.
Children aged 6 to 11 years
In children aged 6 years and over, asthma can be diagnosed with certainty, as identifying reversible expiratory airflow limitation using spirometry becomes more feasible, and the incidence of other early childhood wheeze phenotypes has reduced by this age. In children aged 5 years, the feasibility of spirometry is generally above 85%.43
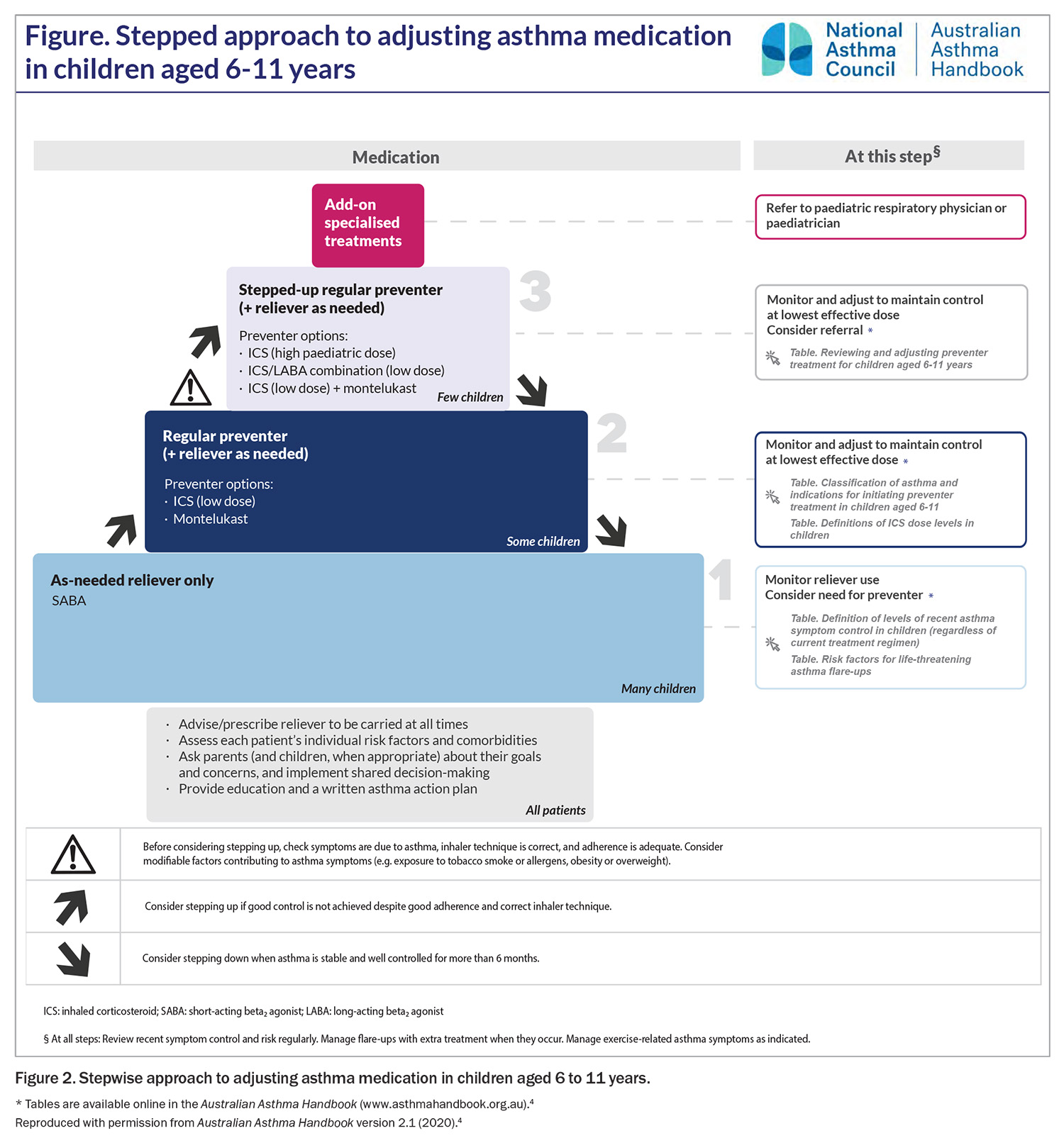
The stepwise approach to maintenance treatments for children aged 6 to 11 years is shown in Figure 2. For children of all ages, the aim of maintenance asthma preventer therapy is to achieve good control of asthma symptoms at the lowest step necessary. Good control of asthma symptoms is considered as:
- infrequent daytime symptoms (two days a week or less)
- no nocturnal symptoms
- no limitation on play, physical activity or school attendance.4
Before any increase in preventer therapy, clinicians should ensure the diagnosis of asthma is correct, as well as assess family and patient understanding, adherence and comorbidities, and minimise exposure to triggers, as described above for children aged 1 to 5 years.
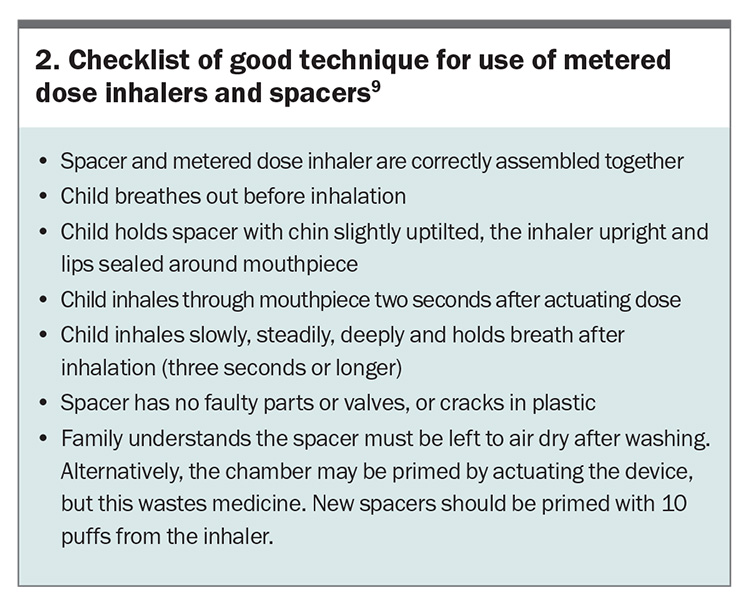
A pressurised metered dose inhaler (pMDI) and spacer is an appropriate first choice for most children.45 pMDI via spacers and nebulisers are equally effective means of delivering beta2 agonists to children with acute asthma. Ongoing parental supervision of medication dosing remains important for school-aged children as they are unlikely to use their devices correctly without careful training and repeated checking of their technique.44 Asking the child to demonstrate how they use their metered dose inhaler and spacer can offer useful insights into the family’s retention of asthma education and home practices. A useful checklist to detect the most common errors in use of metered dose inhalers and spacers is shown in Box 2.9
Leukotriene receptor antagonist vs inhaled corticosteroid
An ICS is recommended as the first-line preventer in Step 2 of the asthma management algorithm for children aged 6 to 11 years. This is based on comparative trials favouring ICS over LTRAs for greater efficacy, symptom reduction, exacerbation prevention and lung function improvement.46,47 However, an LTRA may be more effective for some patients, and some may find adherence to LTRAs easier than to ICS.48,49
Inhaled corticosteroids
At higher doses, ICS have been shown to have a relatively flat dose-response curve, with increasing systemic side effects such as adrenal suppression at doses over 400 mcg/day fluticasone propionate equivalent, without increased efficacy.50 A 2004 Cochrane review suggested that commencing an ICS at a moderate dose is as effective as commencing it at a high dose and then reducing the dose while monitoring symptoms.51
Growth suppression due to ICS is dose-dependent, and different age groups differ in their susceptibility to growth effects, with children aged 4 to 10 years being more susceptible than pubertal children.52 A randomised placebo-controlled trial of ICS in children aged 5 to 13 years reported a mean decrease of about 1 cm in height, typically with onset within two years, that was sustained at follow up through to adulthood.53 In children with persistent asthma requiring maintenance ICS treatment to achieve good asthma control, we recommend that this small effect on final adult height should be viewed as an acceptable trade-off for better asthma control.
The latest GINA recommendations suggest a low threshold for commencing ICS, as a preventer, in children, even for those with infrequent SABA. If not daily ICS then to commence for the duration salbutamol is used. There is no direct paediatric evidence for this approach but is extrapolated from benefit in reducing severe exacerbations in adolescents and adults.
Leukotriene receptor antagonists
LTRAs are effective for exercise-induced bronchoconstriction, with studies in both adults and children reporting a better response than to other options, including ICS and ICS plus LABA. Patients with exercise-induced bronchoconstriction tend to have a smaller drop in expiratory airflow during exercise and a better response to SABA after exercise when using LTRAs compared with combination ICS plus LABA.54-57
An important aspect to discuss openly with parents from the start of LTRA treatment is the potential for neuropsychiatric adverse drug reactions. These have been of concern and have attracted media attention, and are more common in children than adults. The most common adverse reactions include aggression and sleep disorders in younger children and headaches and depression or anxiety in adolescents.58,59 A retrospective cohort study in children reported the onset of neuropsychiatric adverse drug reactions usually within the first two weeks of commencing an LTRA; treatment cessation was not typically required but led to resolution in those who chose to cease.60 Clinicians should be aware of these associations, discuss them openly with parents and be vigilant for adverse events.
Individual responses to Step 3 treatment
Step 2 treatment with an ICS alone is effective in the vast majority of children with mild persistent asthma.61 In children with poor symptom control despite a low-dose ICS (250 mcg/day fluticasone proprionate equivalent or less), where adherence is considered appropriate, there are several options for treatment escalation. These include a high-dose ICS (500 mcg/day fluticasone proprionate equivalent or more), a combination LABA with low-dose ICS or an ICS plus LTRA.
These three treatment options were compared in a prospective, crossover blinded randomised trial in children aged 6 to 18 years with asthma inadequately controlled by a low-dose ICS (twice daily 100 mcg fluticasone proprionate equivalent).62 Patients were randomly allocated to high-dose ICS (twice daily 250 mcg fluticasone proprionate equivalent), low-dose ICS plus LABA or low-dose ICS plus LTRA in a sequential manner. The study results showed that the optimal treatment differed between individual children. ICS plus LABA therapy was significantly more likely to provide the best response (compared with high-dose ICS or ICS plus LTRA). However, as the composite outcome measure included any improvement in FEV1, and inclusion criteria included a demonstrable FEV1 response to a bronchodilator, the study design may have favoured LABA-containing medications.
These findings highlight the need to consider alternatives in Step 3 of the stepwise management algorithm when asthma control is not achieved despite optimal adherence and education. Other factors such as cost may influence decisions. Currently, LTRA is not PBS-subsidised for patients aged over 15 years, although it may be within financial reach of families as generic montelukast options recently became available.
Adolescents aged 12 to 18 years
The prevalence of asthma declines from about 16% in primary school-aged children to 11% in adolescents.63 The management of asthma during adolescence involves navigating challenges as the young person learns to take responsibility for their own health. It is widely accepted this period is associated with reduced compliance with daily asthma medications.64 Concern of side effects, decreased parental supervision and peer approval are contributors to this observation.65 This leads to the management of asthma becoming more challenging due to under-recognition of symptoms, erratic self-medication (i.e. decreased adherence), denial of disease severity and risk-taking behaviours.66
Preventing asthma deaths
Asthma mortality in Australia remains higher than in other comparable developed countries such as Canada, France, Japan and Italy.13 Adolescents are over-represented among asthma deaths, comprising up to 60% of cases.13,14
Recent audits of asthma deaths from the UK and Australia, triggered by increasing concern over preventable and escalating mortality, describe children with a pattern of excessive use of reliever medication and underfilled prescriptions for preventer medications, a history of hospital presentations with poor follow-up care, repeated courses of OCS and frequent missed school days.13,14,67,68 Children from vulnerable families are prominent among paediatric asthma deaths, with high rates of family breakdown, parental substance abuse, domestic violence and child protection involvement.13
Damningly, the UK national review of asthma deaths reported that 46% of deaths could have been avoided if patients had been better managed in the year before they died.66 Patients did not receive key areas of routine care, with only 4% managed in line with current national guideline recommendations. Prescribing errors were widespread, acute asthma was poorly managed, and severe cases were not referred to specialist centres.
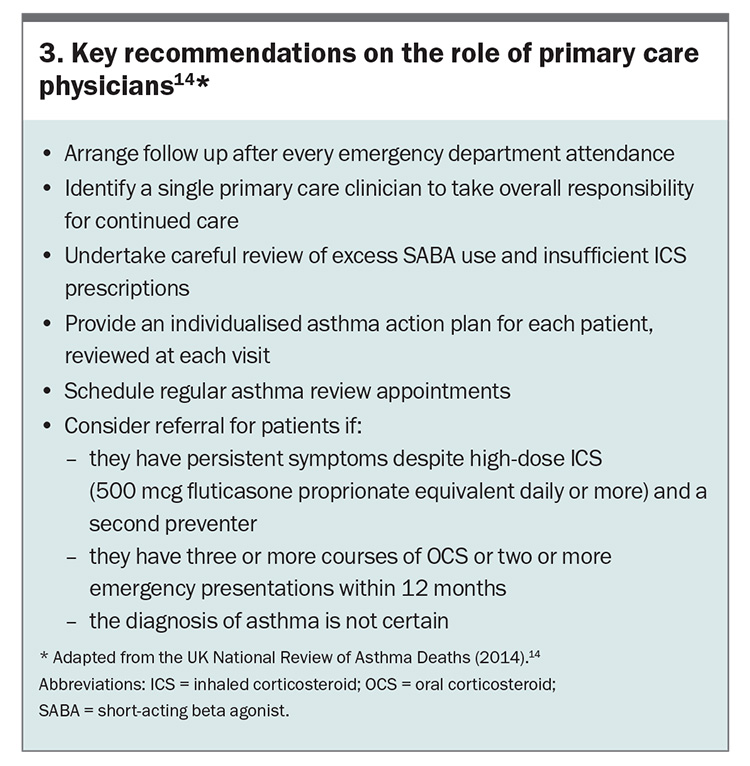
Leading physicians have advocated for a frameshift in the perception of asthma exacerbations, arguing that each acute exacerbation episode should be viewed as a significant marker of poorly controlled disease and prompt a careful review of management.11 Acute asthma attacks carry a risk of further attacks and death. The AAH currently encourages clinicians to increase disease monitoring around these flare-ups and to refer patients with more than one emergency visit in a year or repeated OCS treatments to a specialist centre.4 Recommendations about the key role of primary care physicians from the UK National Review of Asthma Deaths are shown in Box 3.14
SMART: Single Maintenance and Reliever Treatment
The underuse of preventer medication and overuse or reliance on SABA treatment has emerged as a key issue in asthma management. The shift away from using SABA only for mild asthma in paediatrics stems from two areas of concern. Firstly, 30-40% of severe exacerbations arise from patients with ‘Mild’ asthma.69 Secondly adult data reports SABA-only therapy is associated with increased risk of asthma exacerbations.
The 2019 GINA report raised serious concerns about the overuse of SABA reliever treatments paired with the underuse of ICS preventer treatment among adolescents and other age groups. The 2023 guidelines go further to recommend the ICS-formoterol preventer as reliever recommendation to be the first line management approach. This treatment simplifies management, avoids SABA overuse without concomitant ICS administration and is also suitable as a step down approach from patients whose asthma is well controlled on regular ICS or LTRA.
Four studies have evaluated an as needed combination ICS + fast onset LABA in mild asthma. Together these studies include near 10,000 patients (adults and adolescents) and show ICS + formoterol to be superior to as needed SABA + daily ICS treatment, for symptom control and is more effective in exacerbation prevention.70-73 Adolescent specific insight comes from a post-hoc pooled analysis of the SYGMA 1 and 2 trials performed including only those aged between 12 and 18 years. The authors reported no difference in severe exacerbation rate comparing maintenance ICS vs as needed ICS+LABA, however ICS+LABA as needed was associated with reduced median steroid exposure and improved linear growth.74 The results of this study are a useful insight to support SMART as a treatment option for adolescents, however, the study does not demonstrate this to be a superior option in regards to severe exacerbation rate, FEV1 pre bronchodilator and symptom control. Caution should be shown in adopting this approach universally and abandoning daily ICS preventer therapy for adolescents.75
The SMART treatment approach was previously only recommended in children >12 years; the GINA guidelines now include this treatment approach as an alternative to daily preventer and as needed reliever strategy in the 5-11 year age groups. The latest Australian guidelines have adopted the SMART recommendation as a treatment strategy for adolescents and adults but not as a routine approach for younger children. There is a lack of high grade evidence in younger patients and little data on the pharmacokinetics and pharmacodynamics of LABAs in younger children. Further research could evaluate the adequacy of extrapolating from older age groups.76
GINA guidelines advocate children and adolescents should receive an ICS whenever a SABA is required, either as a separate ICS inhaler alongside SABA or using combination ICS plus formoterol (a fast-onset LABA). Only patients using SABA once per month or less need not use an ICS.77 This recommendation is in part derived from large, randomised trials mostly in adults, with some adolescent representation, comparing standard treatment with combination ICS plus fast-onset LABA. In these studies, the ‘maintenance and reliever therapy’ (MART) approach was shown to reduce rates of severe exacerbations and overall ICS dosing.70,78,79
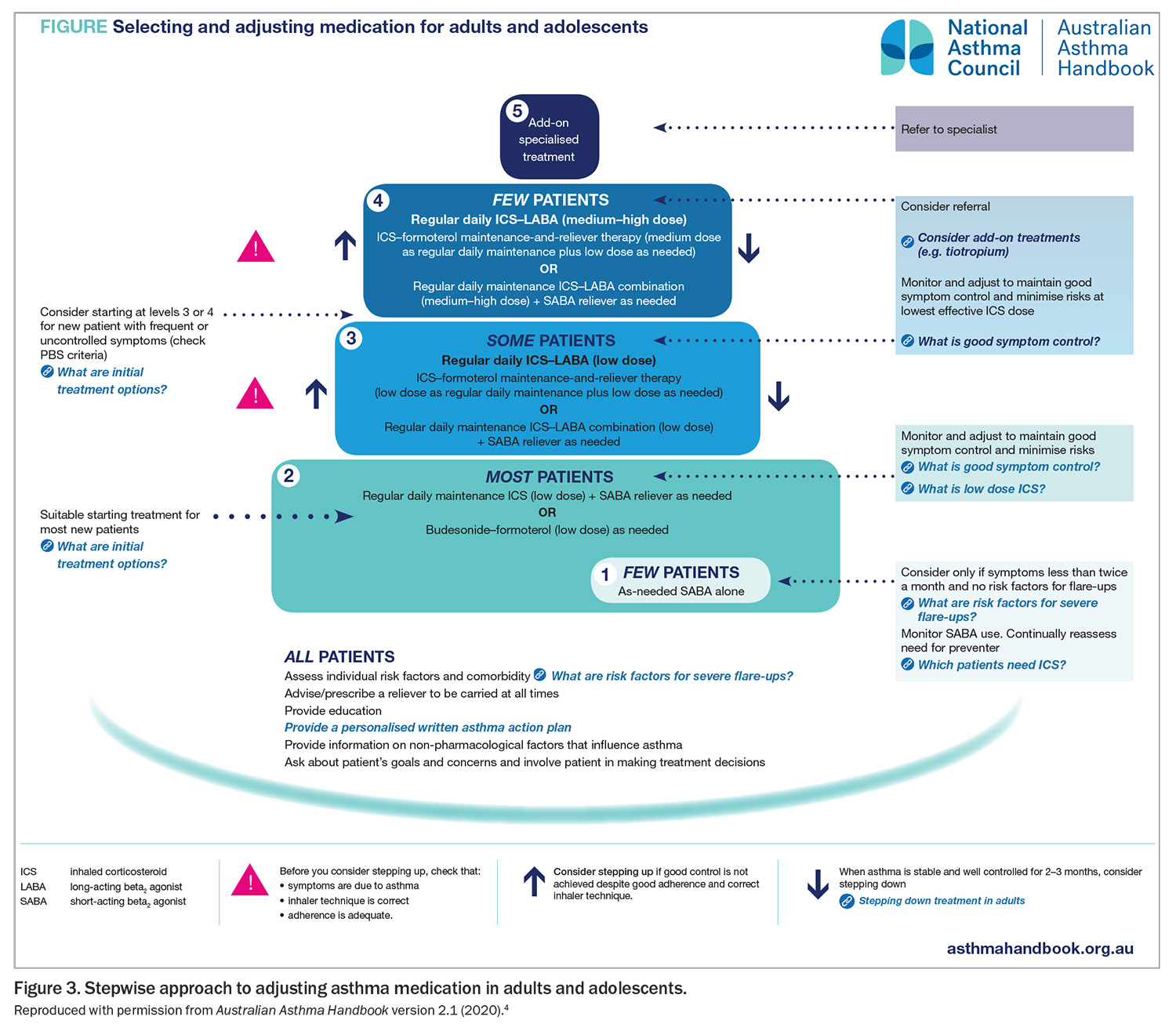
The AAH reviewed its recommendations in response to these GINA guidelines and released a minor update in September 2020 (version 2.1). This includes revised recommendations for adolescents (Figure 3).
In Australia, the PBS provides access to combination budesonide plus formoterol for children aged ≥12 years for step 2 treatment, or younger if management is directed by a respiratory physician or paediatrician. Also, only an ICS plus fast-onset LABA combination (budesonide and formoterol) is suitable for this approach; other ICS plus LABA combinations (e.g. salmeterol and vilanterol) are not to be used for this indication.
Other important management aspects across age groups
Stepping down asthma treatment
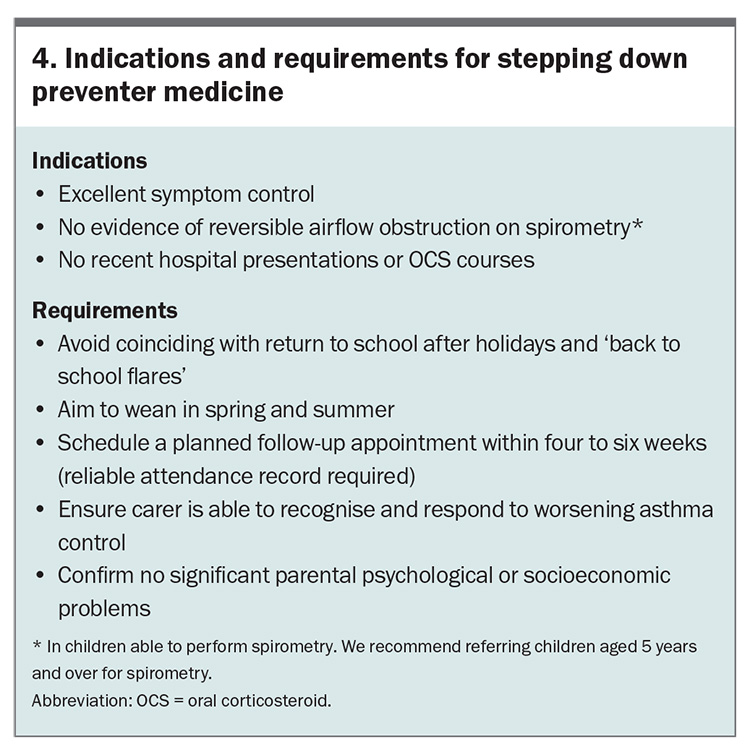
Asthma is considered well controlled when symptoms are absent or mild, occur during the daytime only and quickly respond to a SABA (used less often than twice per week). The patient should have no limitations on play, sport or school attendance, no nocturnal symptoms (AAH) and no recent history of exacerbations managed with OCS or hospitalisation. The indications for step down of asthma preventer medicines are listed in Box 4.
In patients prescribed ICS plus an additional non-ICS preventer (montelukast, combination ICS with LABA, or a biologic agent), a reduction in ICS dosing while maintaining the other preventer has superior outcomes compared with weaning onto ICS alone. This suggests that tapering ICS dosage by 50% before LABA or LTRA discontinuation may be a preferable approach. Seasonal effects are noted, with greater success in spring and summer than at other times.80 There is a lack of data to guide the rate of reduction, and the lowest dose of ICS needed to control asthma and any reduction needs to consider the individual’s potential for exacerbation, the severity of previous exacerbations and the carer’s ability to manage such an occurrence.
Parent education and asthma plans
The provision of an asthma action plan is not only an important clinical communication between care providers and families but also an important opportunity for focused education. Indeed, research suggests that it is not the asthma plan per se but the education that accompanies it that is associated with better disease control.81 Important aspects for clinicians to address include the pathophysiology of the child’s disease, the use and role of reliever and preventer medicines, expectations of treatment and the threshold for medical review.82 Children provided with education and written action plans have been shown to have significantly fewer asthma exacerbations, OCS prescriptions, loss of school days, nocturnal wakenings and overall symptom scores.81,83
School plans
Schools are importantly placed to support the management of children with asthma. The Asthma Friendly Schools Initiative from North America suggested the development of resources for schools to improve awareness of asthma-related issues and a standardised approach to handling worsening asthma in a child.84 Schools should have an annual process for identifying students with asthma, ensure easy access to inhalers (preferably carry their own), identify and reduce common asthma triggers within the environment and support communication and collaboration between carers, students, educators and healthcare workers.84,85 Asthma education for school staff increases asthma knowledge and preparedness.86 It is important that teachers receive guidance and training in appropriate asthma care. Schools should also encourage a policy of exercise for all students with asthma.86,87
Clinicians should be aware of the phenomenon of back-to-school asthma flare-ups; each year, emergency department presentations and hospitalisations surge during the first months of the school year.88 It is important that clinicians recognise the start of the school term as a time to avoid stepping down treatment.4 It is also helpful to plan reviews toward the end of the school holidays, which ensures the opportunity to review and update the asthma action plan and encourage children to communicate their symptoms to teaching staff with the support of their parents.
Medication adherence
Barriers to medication adherence in school-aged children include a lack of motivation, difficulties remembering and social barriers. Children report the paradox that they find parental reminders annoying but that prompting improves adherence.77
It is important to provide practical support to families by openly and compassionately exploring the understanding and obstacles to treatment, and where possible offering strategies to overcome these challenges. Evidence-based strategies to promote adherence include:
- the use of rewards to reinforce adherence
- including treatment within other routines (e.g. mealtime, brushing teeth)
- determining reasonable, specific goals defined by the patient
- using visual or auditory reminders
- using a measure of adherence to benchmark achievement at home
- simplifying treatment regimens (e.g. prescribing once-daily ICS for children aged 12 years and over).89-91
Monitoring devices
Electronic monitoring devices can be fitted to a range of inhalers, and the data downloaded remotely to provide a clear picture of adherence and how it impacts on asthma control and exacerbations. This technology may be useful in children with persistent symptoms and difficulties understanding treatment adherence, to avoid unnecessary investigations or overtreatment.92 Currently, these devices are typically used only by tertiary centres for patients with more severe asthma, but pharmaceutical companies are starting to offer them alongside medications to the broader community.
The development of smartphone apps to support adherence is an emerging area. The opportunity exists for digital media to detail symptom scores, medication adherence information and even basic measures of lung function and to communicate these directly to healthcare providers.94 Studies in adults with asthma found that the use of mobile apps improved medication adherence and asthma control.93 The issues with app development include the profit motives of developers that are placed ahead of the health needs of users. In addition, there is an oversupply of low-quality information apps that either are not effective or do not meet patient needs, or that fail to comply with existing evidence-based clinical practice.95
Complex asthma and the role of biologic agents
An estimated 5 to 10% of children with asthma remain symptomatic despite receiving large amounts of asthma preventer treatment.96,97 Problematic severe asthma (PSA) is the umbrella term used to describe all children who present with ongoing persistent symptoms or frequent attacks despite high-intensity treatment.98 It is felt to comprise of three subgroups of children:
1. Severe therapy-resistant asthma; cases who continue to have poor control, or become uncontrolled with reduction in treatment, once modifiable factors have been identified and addressed (e.g. adherence, reduction in allergen exposure, or treatment of comorbidities). It is recommended these children are phenotypically characterised and assessed as to their eligibility for biologic treatment;
2. Difficult-to-treat asthma in which modifiable factors are the cause of poor control, and once corrected, treatment can be weaned to the lowest possible dose to maintain good asthma control. In this cohort management of treatable traits is a key strategy in symptom control; and finally,
3. Refractory difficult asthma despite identification and correction of modifiable factors disease remains intractable, due to additional factors, including but not limited to psychosocial issues such as safeguarding concerns, an adverse home environment, poor parental supervision, or comorbidities such as obesity, which are largely beyond the control of the child. The increased risk of severe, life-threatening asthma attacks in this subgroup means that consideration for biological therapy is also justified.98
Although patients with PSA represent a small proportion of those with asthma overall, they consume a high proportion of healthcare resources.94
Management of problematic severe asthma
Patients with PSA require a systematic approach that:
- confirms the diagnosis and the contribution of asthma to symptoms
- identifies barriers to effective treatments
- manages comorbidities (anxiety, obesity, vocal cord dysfunction, gastro-oesophageal reflux, allergy and rhinosinusitis)
- optimises treatment and monitors for adverse effects.98
Within complex asthma clinics, this care is coordinated by a respiratory physician in conjunction with some or all of: an asthma nurse specialist, allergy and immunology physician, respiratory scientist, psychologist, physiotherapist, speech pathologist and ear, nose and throat surgeon.99 This multidisciplinary approach is starting to emerge within tertiary paediatric institutions with encouraging evidence of benefit for important outcomes such as rates of exacerbation, hospitalisation and oral corticosteroid exposure.100
Severe asthma is considered in patients with a confirmed asthma diagnosis, comorbidities, optimal adherence and a continued need for high-dose ICS plus a second preventer to maintain control or asthma that remains uncontrolled despite this therapy.85 Children with severe asthma have poor quality of life, limitations on activities and frequent asthma attacks and are at high risk of treatment side effects.101,102
Biological agents indications and limitations
Severe asthma is recognised as a heterogeneous condition, and cohort studies have begun to define phenotypes within this patient group that may allow effective biomarker-driven treatments. The best described phenotypes include allergic and eosinophilic types. Described according to the pattern of inflammatory response. Although no specific phenotypes are agreed on, there appears to be a clustering of an early-onset allergic phenotype, a later-onset obese (primarily female) phenotype and a later-onset eosinophilic phenotype. Identifying eosinophilic inflammatory biomarkers is helpful in considering targeted therapy such as biological agents.103-108
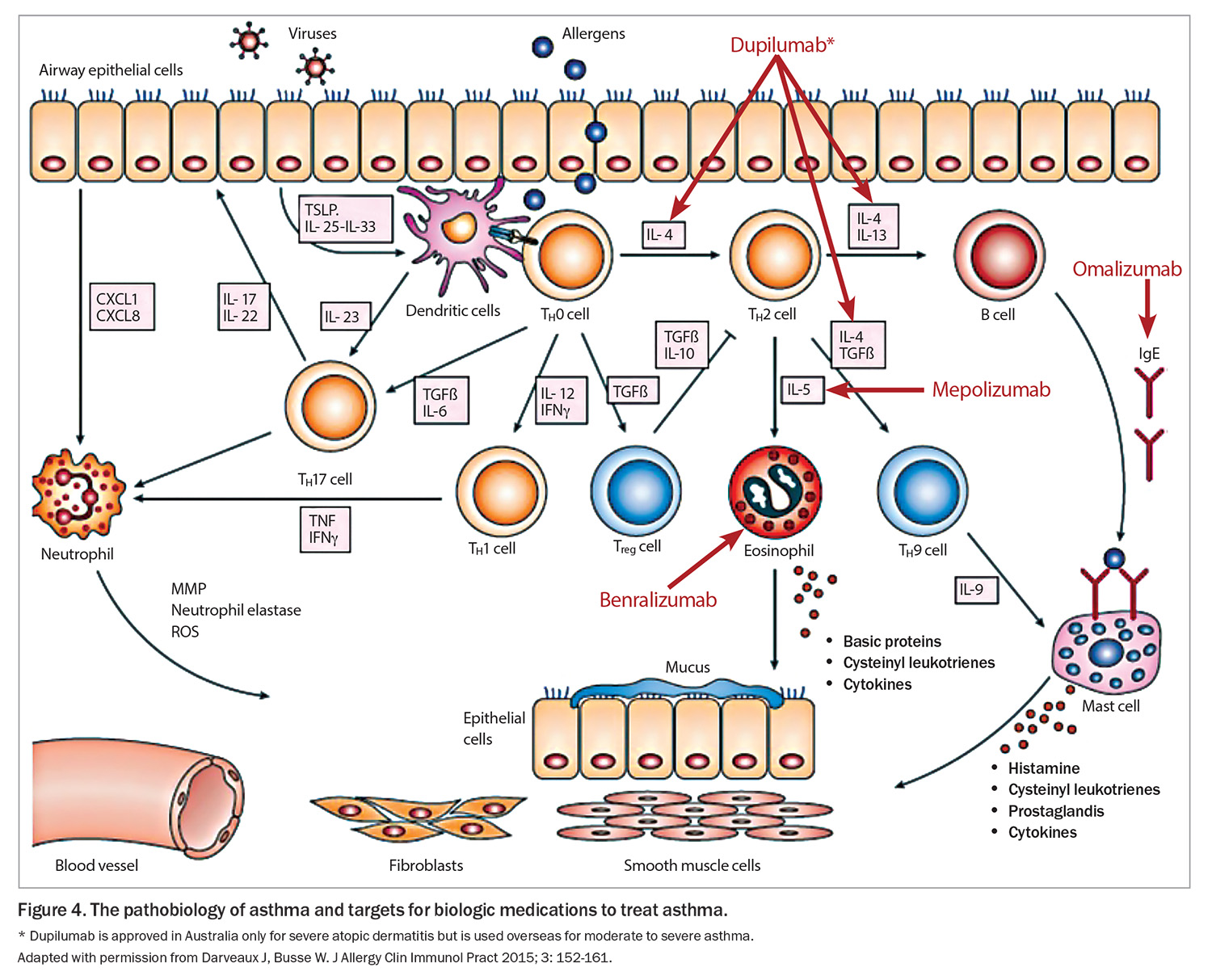
Traditional asthma medications broadly aimed to reduce airway inflammation and reverse bronchoconstriction. Biologic medications now offer a targeted and personalized treatment approach. Measured against placebo, the biologic agents have demonstrated reductions in severe exacerbation rate (about 50%), corticosteroid use, lung function and health related quality of life.101-106
In Australia, the following monoclonal antibody treatments are approved for the treatment of severe asthma:
- Omalizumab: antisoluble IgE, prevents IgE binding to mast cells, which has been used since 2002 for the treatment of uncontrolled severe asthma and has been approved for children aged ≥6 years from 2016, administered subcutaneously two- to four-weekly
- Benralizumab: antibody directed to interleukin-5 receptor, expressed on eosinophils and basophils reducing the production and survival of eosinophils, available for adolescents aged ≥12 years, administered subcutaneously four-weekly, then progressed to eight-weekly
- Mepolizumab: antisoluble interleukin-5, reducing the production and survival of eosinophils, available for adolescents aged ≥12 years, administered subcutaneously four-weekly
- Dupilimab: antibody directed to soluble interleukin-4 and -13, approved for the management of severe asthma and atopic dermatitis (separate indications) in children aged ≥12 years and ≥6 years for atopic dermatitis
- Tezepelumab: antithymic stromal lymphopoietin, indicated for any asthma subtype for adolescents ≥12 years (not currently approved in Australia)
The complex inflammatory cascade of asthma and site of action of these agents is shown in Figure 4.
Treatment algorithms include certain biomarkers to inform the choice of biological agents. Key markers include blood eosinophil count, serum IgE and measured exhaled nitric oxide. These indices have been extrapolated from the inclusion criteria of the placebo controlled trials. To be eligible for a PBS subsidy for monoclonal antibody treatment, patients must be known to a respiratory specialist or severe asthma clinic and meet specified biomarker and clinical criteria.4
The short-term safety profiles are generally excellent for the biologics. The most common reaction being local injection site reactions. Specific agents are associated with other mild adverse effects. Serious rare adverse effects including anaphylaxis and polyangitis are reported and should be monitored for depending on the specific agent used. Long term safety data is lacking, specifically concerning the effect on the developing immune system, vaccine responsiveness and the possible emergence of antidrug antibodies.
Comparative effectiveness and optimal choice is unknown, there have been no RCTs directly comparing asthma biologics for efficacy and safety. The TREAT trial is a UK industry independent RCT comparing mepolizumab and omalizumab for severe paediatric asthma (https://doi.org/10.1186/ISRCTN12109108).
Conclusion
Management recommendations for paediatric asthma vary by age. However, important principles, such as accurate diagnosis and titration of treatment to maintain adequate control at the lowest preventer medication dose, are applicable to all age groups. Patients with well-controlled asthma should have little need of reliever medication, no limitations on activity and no nocturnal symptoms; this should be the goal for the primary physicians of all patients with asthma. Routine review of patients with well-controlled asthma should focus on revising action plans and reinforcing treatment adherence and drug delivery technique. Patients who have poor day-to-day symptom profiles, require more than one course of OCS per year or are not responding to guideline-recommended treatment must be recognised as a concern and referred for specialist assessment and reviewed more regularly.
Recent asthma mortality reviews have identified important risk factors, such as over-reliance on reliever and underuse of preventer medications. Worryingly, UK research suggests that these patients are not being well identified in primary care. Asthma deaths remain highly preventable, and better recognition of at-risk groups and improved adherence to current management guidelines, such as those outlined in the AAH, is crucial to efforts to reduce asthma mortality. Options to improve adherence are increasing, including once-daily administration options for ICS and ICS plus LABA, asthma-focused apps and electronic monitoring devices. For patients with difficult-to-treat asthma and severe asthma, the armamentarium is expanding with novel biological agents targeted against precise disease pathways. Understanding of how best to identify the phenotypes most likely to respond is improving.
In an article entitled ‘After asthma – redefining airway disease’ several thought-provoking recommendations were made.109 Asthma should be considered an umbrella term, encompassing a collection of distinct airway disease phenotypes alongside comorbidities that may contribute to symptoms. Better appreciation of these components and the developmental trajectories of airway disease will allow clinicians to tailor an individualised approach to asthma management for each patient, trialling and evaluating therapies that have led to a clinical improvement, or not, and considering the treatment of comorbidities that influence disease or influence the perception of symptoms. Lastly, clinicians must adopt a ‘zero tolerance’ approach toward asthma attacks, recognising them as a ‘red flag’, if future efforts to reduce the unacceptable ongoing asthma mortality are to be successful. RMT
COMPETING INTERESTS: None.
References
1. AIHW. Asthma [web report]. Canberra: AIHW; 2019.
2. Acworth J, Babl F, Borland M, et al. Patterns of presentation to the Australian and New Zealand Paediatric Emergency Research Network. Emerg Med Australas 2009; 21: 59-66.
3. Hiscock H, Roberts G, Efron D, et al. Children Attending Paediatricians Study: a national prospective audit of outpatient practice from the Australian Paediatric Research Network. Med J Aust 2011; 194: 392-397.
4. National Asthma Council Australia. Australian asthma handbook, version 2.1. Melbourne: National Asthma Council Australia; 2020. Available online at: www.asthmahandbook.org.au (accessed August 2020).
5. Global Initiative for Asthma (GINA). 2023 GINA Main Report. Fontana, WI: GINA; 2023. Available online at: https://ginasthma.org/2023-gina-main-report/ (accessed May 2024).
6. Braithwaite J, Hibbert PD, Jaffe A, et al. Quality of health care for children in Australia, 2012-2013. JAMA 2018; 319: 1113-1124.
7. Cloutier MM, Salo PM, Akinbami LJ, et al. Clinician agreement, self-efficacy, and adherence with the guidelines for the diagnosis and management of asthma. J Allergy Clin Immunol Pract 2018; 6: 886-894.e4.
8. Rance K, O’Laughlen M, Ting S. Improving asthma care for African American children by increasing national asthma guideline adherence. J Pediatr Health Care 2011; 25: 235-249.
9. Srour-Alphonse P, Cvetkovski B, Rand CS, et al. It takes a village - asthma networks utilized by parents when managing childhood asthma medications. J Asthma 2020; 57: 306-318.
10. van Asperen P, Robinson P. Age-specific management of asthma in children. Med Today 2014; 15(9): 14-28.
11. Bush A, Kleinert S, Pavord ID. The asthmas in 2015 and beyond: a Lancet Commission. Lancet 2015; 385: 1273-1275.
12. Ebmeier S, Thayabaran D, Braithwaite I, Bénamara C, Weatherall M, Beasley R. Trends in international asthma mortality: analysis of data from the WHO Mortality Database from 46 countries (1993-2012). Lancet 2017; 390: 935-945.
13. Fitzgerald DA, Gillis J. Asthma deaths in children in New South Wales 2004-2013: Could we have done more? J Paediatr Child Health 2015; 51: 1127-1133.
14. Levy ML. National review of asthma deaths (NRAD). Br J Gen Pract 2014; 64: 564.
15. Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ. Asthma and wheezing in the first six years of life. The Group Health Medical Associates. N Engl J Med 1995; 332: 133-138.
16. Martinez FD. What have we learned from the Tucson Children’s Respiratory Study? Paediatr Respir Rev 2002; 3: 193-197.
17. Castro-Rodriguez JA, Cifuentes L, Rodríguez-Martínez CE. The asthma predictive index remains a useful tool to predict asthma in young children with recurrent wheeze in clinical practice. J Allergy Clin Immunol 2011; 127: 1082-1083.
18. Brand PL. The Asthma Predictive Index: not a useful tool in clinical practice. J Allergy Clin Immunol 2011; 127: 293-294.
19. Reyna ME, Dai R, Tran MM, et al. Development of a symptom-based tool for screening of children at high risk of preschool asthma. JAMA Netw Open 2022; 5: e2234714.
20. Marlow R, Finn A, Henderson J. Assessing the association between bronchiolitis in infancy and recurrent wheeze: a whole English birth cohort case-control study. Thorax 2019; 74: 503-505.
21. Drysdale SB, Cathie K, Flamein F, et al. Nirsevimab for prevention of hospitalizations due to RSV in infants. New Engl J Med 2023; 389: 2425-2435.
22. Rosas-Salazar C, Chirkova T, Gebretsadik T, et al. Respiratory syncytial virus infection during infancy and asthma during childhood in the USA (INSPIRE): a population-based, prospective birth cohort study. Lancet 2023; 401: 1669-1680.
23. O’Brien S, Borland ML, Cotterell E, et al. Australasian bronchiolitis guideline. J Paediatr Child Health 2019; 55: 42-53.
24. Yusuf F, Prayle AP, Yanney MP. ß2-agonists do not work in children under 2 years of age: myth or maxim? Breathe (Sheff) 2019; 15: 273-276.
25. Bialy L, Foisy M, Smith M, Fernandes RM. The Cochrane Library and the treatment of bronchiolitis in children: an overview of reviews. Evidence‐Based Child Health 2011; 6: 258-275.
26. Cai Z, Lin Y, Liang J. Efficacy of salbutamol in the treatment of infants with bronchiolitis: A meta-analysis of 13 studies. Medicine (Baltimore) 2020; 99: e18657.
27. Bisgaard H, Hermansen MN, Loland L, Halkjaer LB, Buchvald F. Intermittent inhaled corticosteroids in infants with episodic wheezing. N Engl J Med 2006; 354: 1998-2005.
28. Frey U, von Mutius E. The challenge of managing wheezing in infants. N Engl J Med 2009; 360: 2130-2133.
29. Brand PL, Baraldi E, Bisgaard H, et al. Definition, assessment and treatment of wheezing disorders in preschool children: an evidence-based approach. Eur Respir J 2008; 32: 1096-1110.
30. Bush A. Practice imperfect - treatment for wheezing in preschoolers. N Engl J Med 2009; 360: 409-410.
31. Royal Children’s Hospital Melbourne. Asthma acute. Last updated June 2018. Available online at: www.rch.org.au/clinicalguide/guideline_index/Asthma_acute/ (accessed August 2020).
32. Children’s Health Queensland Hospital and Health Service. Pre-school wheeze - emergency management in children. Available online at: www.childrens.health.qld.gov.au/guideline-preschool-wheeze-emergency-management-in-children/ (accessed August 2020).
33. Panickar J, Lakhanpaul M, Lambert PC, et al. Oral prednisolone for preschool children with acute virus-induced wheezing. N Engl J Med 2009; 360: 329-338.
34. Foster SJ, Cooper MN, Oosterhof S, Borland ML. Oral prednisolone in preschool children with virus-associated wheeze: a prospective, randomised, double-blind, placebo-controlled trial. Lancet Respir Med 2018; 6: 97-106.
35. Zorc JJ. Oral corticosteroids reduce length of hospital stay for preschool children with virus-associated wheeze. Lancet Respir Med 2018; 6: 76-77.
36. Grigg J. Role of systemic steroids in acute preschool wheeze. Arch Dis Child 2010; 95: 491-492.
37. Abrams EM, Becker AB, Szefler SJ. Use of oral corticosteroids in the wheezy toddler. J Pediatr 2018; 201: 16-20.
38. Wassall HJ, Devenny AM, Daud Khan S, Ninan TK, Russell G. A comparison of virus-associated and multi-trigger wheeze in school children. J Asthma 2005; 42: 737-744.
39. Schultz A, Devadason SG, Savenije OE, Sly PD, Le Souëf PN, Brand PL. The transient value of classifying preschool wheeze into episodic viral wheeze and multiple trigger wheeze. Acta Paediatr 2010; 99: 56-60.
40. Wang Z, May SM, Charoenlap S, et al. Effects of secondhand smoke exposure on asthma morbidity and health care utilization in children: a systematic review and meta-analysis. Ann Allergy Asthma Immunol 2015; 115: 396-401.e2.
41. Brand PL, Caudri D, Eber E, et al. Classification and pharmacological treatment of preschool wheezing: changes since 2008. Eur Respir J 2014; 43: 1172-1177.
42. Bacharier LB, Guilbert TW. Diagnosis and management of early asthma in preschool-aged children. J Allergy Clin Immunol 2012; 130: 287-298.
43. Kampschmidt JC, Brooks EG, Cherry DC, Guajardo JR, Wood PR. Feasibility of spirometry testing in preschool children. Pediatr Pulmonol 2016; 51: 258-266.
44. Ram FS, Brocklebank DM, White J, Wright JP, Jones PW. Pressurised metered dose inhalers versus all other hand-held inhaler devices to deliver beta-2 agonist bronchodilators for non-acute asthma. Cochrane Database Syst Rev 2002; (1): CD002158.
45. Kerem E, Levison H, Schuh S, et al. Efficacy of albuterol administered by nebulizer versus spacer device in children with acute asthma. J Pediatr 1993; 123: 313-317.
46. Zeiger RS, Szefler SJ, Phillips BR, et al. Response profiles to fluticasone and montelukast in mild-to-moderate persistent childhood asthma. J Allergy Clin Immunol 2006; 117: 45-52.
47. Castro-Rodriguez JA, Rodrigo GJ. The role of inhaled corticosteroids and montelukast in children with mild-moderate asthma: results of a systematic review with meta-analysis. Arch Dis Child 2010; 95: 365-370.
48. Fitzpatrick AM, Jackson DJ, Mauger DT, et al. Individualized therapy for persistent asthma in young children. J Allergy Clin Immunol 2016; 138: 1608-1618.e12.
49. Ducharme FM, Noya FJ, Allen-Ramey FC, Maiese EM, Gingras J, Blais L. Clinical effectiveness of inhaled corticosteroids versus montelukast in children with asthma: prescription patterns and patient adherence as key factors. Curr Med Res Opin. 2012; 28: 111-119.
50. Gulliver T, Morton R, Eid N. Inhaled corticosteroids in children with asthma: pharmacologic determinants of safety and efficacy and other clinical considerations. Paediatr Drugs 2007; 9: 185-194.
51. Powell H, Gibson PG. High dose versus low dose inhaled corticosteroid as initial starting dose for asthma in adults and children. Cochrane Database Syst Rev 2004; (2): CD004109.
52. Pedersen S. Do inhaled corticosteroids inhibit growth in children? Am J Respir Crit Care Med 2001; 164: 521-535.
53. Kelly HW, Sternberg AL, Lescher R, et al. Effect of inhaled glucocorticoids in childhood on adult height. N Engl J Med 2012; 367: 904-912.
54. Villaran C, O’Neill SJ, Helbling A, et al. Montelukast versus salmeterol in patients with asthma and exercise-induced bronchoconstriction. Montelukast/Salmeterol Exercise Study Group. J Allergy Clin Immunol 1999; 104(3 Pt 1): 547-553.
55. Raissy HH, Harkins M, Kelly F, Kelly HW. Pretreatment with albuterol versus montelukast for exercise-induced bronchospasm in children. Pharmacotherapy 2008; 28: 287-294.
56. Fogel RB, Rosario N, Aristizabal G, et al. Effect of montelukast or salmeterol added to inhaled fluticasone on exercise-induced bronchoconstriction in children. Ann Allergy Asthma Immunol 2010; 104: 511-517.
57. Stelmach I, Grzelewski T, Majak P, Jerzynska J, Stelmach W, Kuna P. Effect of different antiasthmatic treatments on exercise-induced bronchoconstriction in children with asthma. J Allergy Clin Immunol 2008; 121: 383-389.
58. Aldea Perona A, García-Sáiz M, Sanz Álvarez E. Psychiatric disorders and montelukast in children: a disproportionality analysis of the VigiBase(®). Drug Saf 2016; 39: 69-78.
59. Glockler-Lauf SD, Finkelstein Y, Zhu J, Feldman LY, To T. Montelukast and neuropsychiatric events in children with asthma: a nested case-control study. J Pediatr 2019; 209: 176-182.e4.
60. Benard B, Bastien V, Vinet B, Yang R, Krajinovic M, Ducharme FM. Neuropsychiatric adverse drug reactions in children initiated on montelukast in real-life practice. Eur Respir J 2017; 50: 1700148.
61. Arets HG, Kamps AW, Brackel HJ, Mulder PG, Vermue NA, van der Ent CK. Children with mild asthma: do they benefit from inhaled corticosteroids?. Eur Respir J 2002; 20: 1470-1475.
62. Lemanske RF Jr, Mauger DT, Sorkness CA, et al. Step-up therapy for children with uncontrolled asthma receiving inhaled corticosteroids. N Engl J Med. 2010; 362: 975-985.
63. Marks G, Ampon R, Poulos L, Reddel H. Incidence and remission of asthma in Australian children: findings from a population cohort. Eur Resp J 2019; 54 Suppl 63: PA2784.
64. Kosse RC, Koster ES, Kaptein AA, de Vries TW, Bouvy ML. Asthma control and quality of life in adolescents: the role of illness perceptions, medication beliefs, and adherence. J Asthma 2020; 57: 1145-1154.
65. Netz M, Fedele DA, Sweenie R, Baker D, Light M, McQuaid EL. Asthma management responsibility, control, and quality of life among emerging adolescents. J Pediatr Psychol 2020; 45: 40-49.
66. de Benedictis D, Bush A. Asthma in adolescence: Is there any news? Pediatr Pulmonol 2017; 52: 129-138.
67. Carroll W, Clayton S, Frost S, et al. If it’s ‘only’ asthma, why are children still dying? Arch Dis Child 2020; 105: 494-498.
68. Levy ML. The national review of asthma deaths: what did we learn and what needs to change? Breathe (Sheff) 2015; 11: 14-24.
69. Dusser D, Montani D, Chanez P, et al. Mild asthma: an expert review on epidemiology, clinical characteristics and treatment recommendations. Allergy 2007; 62: 591-604.
70. O’Byrne PM, FitzGerald JM, Bateman ED, et al. Inhaled combined budesonide-formoterol as needed in mild asthma. N Engl J Med 2018; 378: 1865-1876.
71. Bateman ED, Reddel HK, O’Byrne PM, et al. As-needed budesonide-formoterol versus maintenance budesonide in mild asthma. N Engl J Med 2018; 378: 1877-1887.
72. Beasley R, Holliday M, Reddel HK, et al. Novel START Study Team. Controlled trial of budesonide-formoterol as needed for mild asthma. N Engl J Med 2019; 380: 2020-2030.
73. Hardy J, Baggott C, Fingleton J, et al. PRACTICAL study team. Budesonide-formoterol reliever therapy versus maintenance budesonide plus terbutaline reliever therapy in adults with mild to moderate asthma (PRACTICAL): a 52-week, open-label, multicentre, superiority, randomised controlled trial. Lancet 2019; 394: 919-928.
74. Reddel HK, O’Byrne PM, FitzGerald JM, et al. Efficacy and safety of as-needed budesonide-formoterol in adolescents with mild asthma. J Allergy Clin Immunol Pract 2021; 9: 3069-3077.
74. Farzan S, Ponda P. What is SMART for some may not be right for all. J Allergy Clin Immunol Pract 2021; 9: 3078-3079.
76. Abrams EM, Shaker M, Greenhawt M, Fernandes RM, Sinha I. Treatment of mild-to-moderate asthma in childhood and adolescence in 2021. Lancet Respir Med 2021; 9: 443-445.
77. Reddel HK, FitzGerald JM, Bateman ED, et al. GINA 2019: a fundamental change in asthma management. Treatment of asthma with short-acting bronchodilators alone is no longer recommended for adults and adolescents. Eur Respir J 2019; 53: 1901046.
78. Jorup C, Lythgoe D, Bisgaard H. Budesonide/formoterol maintenance and reliever therapy in adolescent patients with asthma. Eur Respir J 2018; 51: 1701688.
79. O’Byrne PM, Bisgaard H, Godard PP, et al. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma. Am J Respir Crit Care Med 2005; 171: 129-136.
80. Rogers L, Reibman J. Stepping down asthma treatment: how and when. Curr Opin Pulm Med 2012; 18: 70-75.
81. Espinoza-Palma T, Zamorano A, Arancibia F, et al. Effectiveness of asthma education with and without a self-management plan in hospitalized children. J Asthma 2009; 46: 906-910.
82. Kelso JM. Do written asthma action plans improve outcomes? Pediatr Allergy Immunol Pulmonol 2016; 29: 2-5.
83. Agrawal SK, Singh M, Mathew JL, Malhi P. Efficacy of an individualized written home-management plan in the control of moderate persistent asthma: a randomized, controlled trial. Acta Paediatr 2005; 94: 1742-1746.
84. Cicutto L, Conti E, Evans H, et al. Creating asthma-friendly schools: a public health approach. J Sch Health 2006; 76: 255-258.
85. Hill RA, Britton JR, Tattersfield AE. Management of asthma in schools. Arch Dis Child 1987; 62: 414-415.
86. Kew KM, Carr R, Donovan T, Gordon M. Asthma education for school staff. Cochrane Database Syst Rev 2017; 4(4): CD012255.
87. Mellis CM, Bowes G, Henry RL, et al. A national policy on asthma management for schools. The Asthma Special Interest Group, Thoracic Society of Australia and New Zealand. J Paediatr Child Health 1994; 30: 98-101.
88. Sears MR. Epidemiology of asthma exacerbations. J Allergy Clin Immunol 2008; 122: 662-668.
89. Penza-Clyve SM, Mansell C, McQuaid EL. Why don’t children take their asthma medications? A qualitative analysis of children’s perspectives on adherence. J Asthma 2004; 41: 189-197.
90. Ezzell K. Strategies to guide medication adherence discussions with parents of children with asthma. Pediatr Nurs 2017; 43: 219-222.
91. Klok T, Kaptein AA, Brand PLP. Non-adherence in children with asthma reviewed: the need for improvement of asthma care and medical education. Pediatr Allergy Immunol 2015; 26: 197-205.
92. Jochmann A, Artusio L, Jamalzadeh A, et al. Electronic monitoring of adherence to inhaled corticosteroids: an essential tool in identifying severe asthma in children. Eur Respir J 2017; 50: 1700910.
93. Kagen S, Garland A. Asthma and allergy mobile apps in 2018. Curr Allergy Asthma Rep 2019; 19: 6.
94. Unni E, Gabriel S, Ariely R. A review of the use and effectiveness of digital health technologies in patients with asthma. Ann Allergy Asthma Immunol 2018; 121: 680-691.e1.
95. Huckvale K, Morrison C, Ouyang J, Ghaghda A, Car J. The evolution of mobile apps for asthma: an updated systematic assessment of content and tools. BMC Med 2015; 13: 58.
96. Fleming L, Murray C, Bansal AT, et al. The burden of severe asthma in childhood and adolescence: results from the paediatric U-BIOPRED cohorts. Eur Respir J 2015; 46: 1322-1333.
97. Nordlund B, Melén E, Schultz ES, Grönlund H, Hedlin G, Kull I. Prevalence of severe childhood asthma according to the WHO. Respir Med 2014; 108: 1234-1237.
98. Pijnenburg MW, Fleming L. Advances in understanding and reducing the burden of severe asthma in children. Lancet Respir Med 2020; 8: 1032-1044.
99. Pike KC, Levy ML, Moreiras J, Fleming L. Managing problematic severe asthma: beyond the guidelines. Arch Dis Child 2018; 103: 392-397.
100. Lieu N, Krishnananthan T, Hatton L, Wong M, Ray R, Mahmood D, Koo S, Pandit C, Towns S, Milne B, Middleton A, Osland K, Kennedy B, Jeyasuriya G, Singh J, Lu M, Field P, Selvadurai H, Fitzgerald D, Marshall T, Robinson P. Impact of a paediatric multidisciplinary complex asthma service on outcomes. Respirology Volume 28, Issue S2, TO054 [Abstract].
101. Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J 2014; 43: 343-373.
102. Grainge CL, Maltby S, Gibson PG, Wark PA, McDonald VM. Targeted therapeutics for severe refractory asthma: monoclonal antibodies. Expert Rev Clin Pharmacol 2016; 9: 927-941.
103. Lanier B, Bridges T, Kulus M, Taylor AF, Berhane I, Vidaurre CF. Omalizumab for the treatment of exacerbations in children with inadequately controlled allergic (IgE-mediated) asthma. J Allergy Clin Immunol 2009; 124: 1210-1216.
104. Brodlie M, McKean MC, Moss S, Spencer DA. The oral corticosteroid-sparing effect of omalizumab in children with severe asthma. Arch Dis Child 2012; 97: 604-609.
105. Ortega HG, Yancey SW, Mayer B, et al. Severe eosinophilic asthma treated with mepolizumab stratified by baseline eosinophil thresholds: a secondary analysis of the DREAM and MENSA studies. Lancet Respir Med 2016; 4: 549-556.
106. Pavord ID, Korn S, Howarth P, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet 2012; 380: 651-659.
107. FitzGerald JM, Bleecker ER, Menzies-Gow A, et al. Predictors of enhanced response with benralizumab for patients with severe asthma: pooled analysis of the SIROCCO and CALIMA studies. Lancet Respir Med 2018; 6: 51-64.
108. Schepel IRM, Banzon TM, Phipatanakul W. Future of biologics in pediatric asthma: optimizing response, early introduction, and equitable access to treatment. Ann Allergy Asthma Immunol 2024; 132: 13-20.
109. Pavord ID, Beasley R, Agusti A, et al. After asthma: redefining airways diseases. Lancet 2018; 391: 350-400.