Screen-detected and incidentally detected lung nodules: a guide for GPs
The Australian National Lung Cancer Screening Program aims to save lives by detecting lung cancer at an earlier stage by screening high-risk individuals using low-dose CT and categorising pulmonary nodules based on their malignancy risk. Patients with high-risk nodules will undergo further evaluation and management according to optimal care pathways for suspected lung cancer. Nodules may also be detected incidentally during CT imaging for other indications.
- The Australian National Lung Cancer Screening Program will begin on 1 July 2025 and aims to detect lung cancer at an earlier stage.
- GPs will be a key point of entry for participants into the program.
- Structured radiology reports will be sent to GPs with recommendations for action.
- Patients with reported high-risk and very high-risk pulmonary nodules should be referred to a respiratory physician or specialist linked with a lung cancer multidisciplinary team.
- Pulmonary nodules may be incidentally detected during CT imaging for other indications.
In Australia, lung cancer is the fifth most common cancer but the leading cause of cancer death.1 The overall five-year survival rate of lung cancer is 26%, and this declines to 11% in Aboriginal and Torres Strait Islander people.1 The Australian National Lung Cancer Screening Program (NLCSP) will begin on 1 July 2025 and aims to save lives by detecting lung cancer at an earlier stage, when it is more likely to be amenable to curative treatment.2,3 GPs will play a key role in the identification of people who are eligible for screening, referral for a low-dose CT (LDCT) scan, discussion of the results and actioning of the recommended next steps.
Identification of eligible individuals for screening
The NLCSP differs from other national population screening programs in that it is targeted to individuals with a high risk of lung cancer. Eligible people will be those aged between 50 and 70 years with no symptoms of lung cancer (such as dyspnoea, chest pain, cough, haemoptysis, non-resolving chest infection or unexplained weight loss). In addition, they must currently smoke or have quit smoking within the past 10 years and have a history of smoking of at least 30 pack-years.4 The NLCSP does not currently include people with other risk factors for lung cancer such as occupational exposures and family history of lung cancer. The NLCSP will be subject to re-evaluation over time.
In the GP clinic, eligible people may be identified by:
- proactive identification, where electronic medical records are audited by the GP or staff at the practice for eligible individuals who are then invited to attend for assessment
- opportunistic identification, where the individual has visited their GP for an unrelated purpose and is concurrently assessed for screening
- self-identification, where the individual seeks specific consultation with their GP regarding screening.
GPs will need to register themselves or their practices with the National Cancer Screening Register (NCSR) if they are not already registered.5 This interface is used for the cervical and bowel cancer screening programs and facilitates submission of participant information and assists with reminders for screening.
Low-dose CT screening
Referral
Participants who are eligible for the NLCSP can then be referred for a screening LDCT at any participating public or private radiology service. In some rural and remote communities, LDCT may be available through the Heart of Australia mobile CT clinics.6
The Australian Government Department of Health and Aged Care is working with key practice software providers to integrate a standardised NLCSP LDCT referral template. This template includes a specific statement that the request is for lung cancer screening, with fields to confirm participant eligibility and to note whether this is a two-yearly scan or shorter interval scan, as well as key information required by the radiologist to interpret the results and assess the malignancy risk of any pulmonary nodules. The referral template also includes details of any previously performed chest CT (necessary to determine if nodules have grown), any family history of lung cancer in a first-degree relative (required for nodule malignancy risk calculation) or personal history of any cancer (as suspected metastases require specific follow-up recommendations).
Categorisation
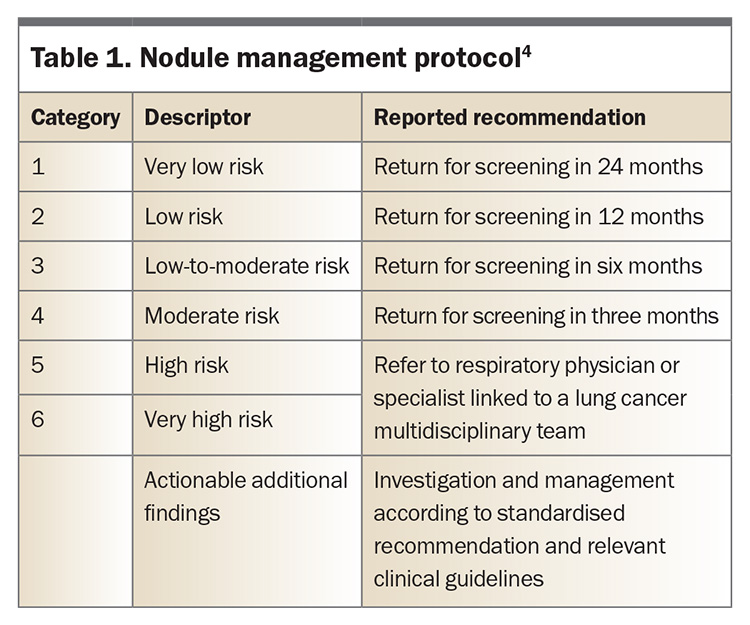
The LDCT results will be reported using the NLCSP Nodule Management Protocol that has been created to guide the management of screen-detected pulmonary nodules. This protocol has been developed in consultation with the Royal Australian and New Zealand College of Radiologists (RANZCR), and the radiology workforce will receive education on it in the lead up to July 2025. By virtue of the higher risk population, nodules detected through screening have a higher risk of malignancy compared with nodules detected incidentally. Screen-detected pulmonary nodules will be classified into one of six categories based on their malignancy risk, from very low through to very high (Table 1). A seventh category (category 0, ‘incomplete’) indicates possible infection requiring specified short-interval follow up.
Radiology report findings
A structured radiology report will be sent to both the referring practitioner as well as the NCSR. The participant will be notified by the NCSR of the recommended next steps. Very low-risk findings do not require immediate action and these participants will remain in the screening program and receive a reminder to see their GP to arrange a repeat scan in two years (Table 1).4 If the scan has low-risk, low-to-moderate risk or moderate-risk findings, the participant will receive a letter from the NCSR advising them to visit their GP to arrange an interval LDCT after 12, six or three months, respectively (Table 1).4 Those with high-risk or very high-risk findings will receive a letter to see their GP to refer them to a respiratory physician or other specialist linked to a lung cancer multidisciplinary team for further evaluation.
It is common for additional findings to be observed on LDCT that are unrelated to lung cancer (e.g. coronary artery calcification or emphysema), and such findings will have standardised suggested actions for GPs. Guidelines for actionable additional findings will be outlined in the forthcoming NLCSP guidelines. Some findings may require specialist input, and patients with other findings may be managed in primary care, according to usual care recommendations.
High-risk or very high-risk screen-detected pulmonary nodules
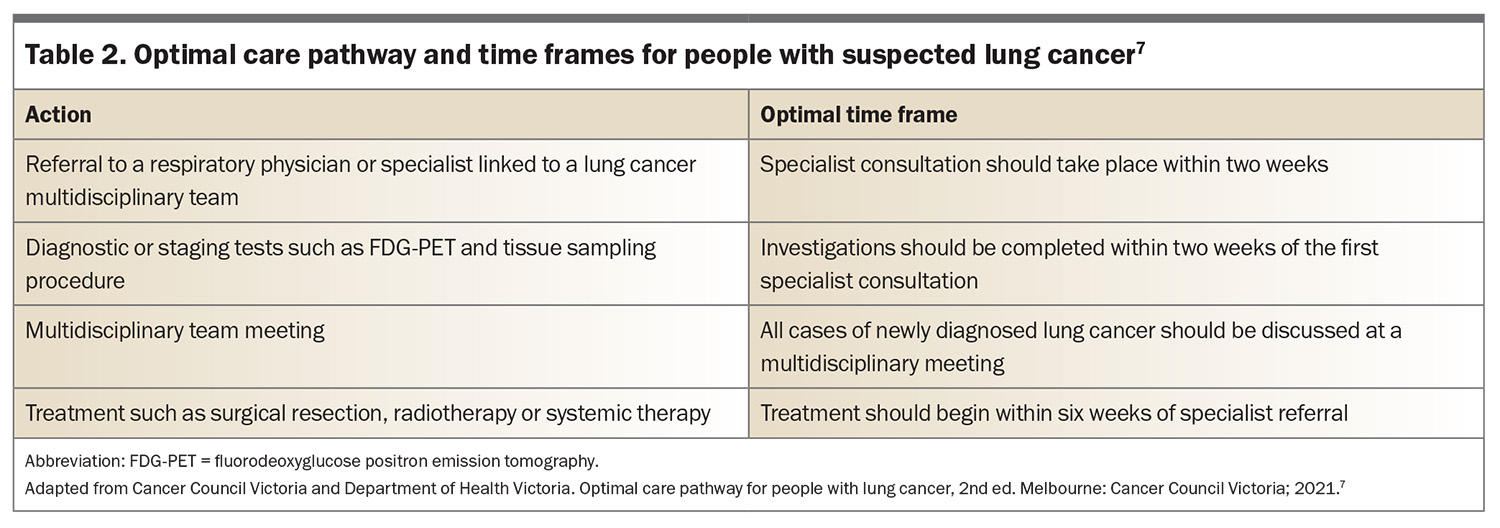
In cases where a high-risk or very high-risk pulmonary nodule is detected on LDCT and the patient is referred to a respiratory physician or specialist linked to a lung cancer multidisciplinary team, the participant will undergo further evaluation and management according to optimal care pathways for suspected lung cancer.7 The optimal care pathway recommendations inform best-quality practice delivered within optimal time frames (Table 2).7 These have recently been complemented by Australasian lung cancer clinical quality indicators, which provide measures of best-practice outcomes.8 Multidisciplinary care for people with lung cancer is recognised as the gold standard (regardless of stage), with a measurable survival benefit.9 Sources of information on locations and referral pathways to lung cancer multidisciplinary teams are in development. In NSW and the ACT, search tools such as Canrefer may facilitate this process (https://www.canrefer.org.au).
Incidentally detected pulmonary nodules
With the rise of thoracic CT imaging for nonpulmonary nodule indications, there has been an increase in incidentally detected pulmonary nodules, which have a prevalence of malignancy of about 5%.10,11 This highlights the importance of appropriate management of incidentally detected pulmonary nodules. In contrast to screen-detected nodules, evaluation of an incidentally detected nodule requires additional clinical context to determine the probability of malignancy and to guide next steps, with prior imaging and nodule behaviour paramount in this.12
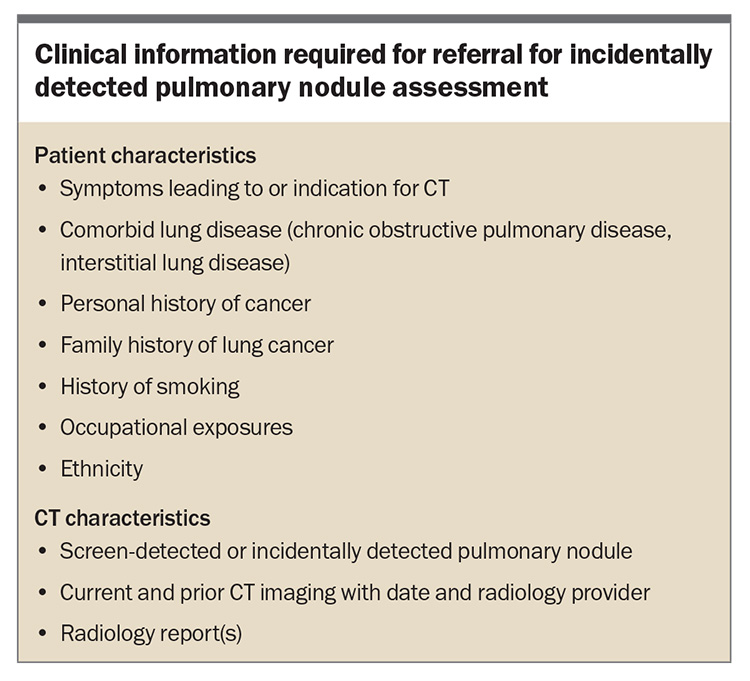
The Thoracic Society of Australia and New Zealand (TSANZ), in collaboration with the Australian and New Zealand Society of Thoracic Radiology (ANZSTR), is anticipated to release a practical guide for clinicians on the management of screen-detected and incidentally detected pulmonary nodules. For GPs, the minimum clinical information required for a referral to a respiratory physician or specialist linked to a lung cancer multidisciplinary team is outlined in the Box. Many centres are now developing specific lung nodule evaluation teams to meet the rising demand for screen- and incidentally detected nodule evaluation.
Importance of smoking cessation approaches
Tobacco smoking continues to be the foremost modifiable risk factor for lung cancer. There is clear evidence that participants in lung cancer screening programs have higher cessation rates than those expected in the general population.13 The NLCSP is targeted to people with a current heavy smoking history, and enrolment in screening represents an opportunity to offer smoking cessation advice and support.14 The guideline includes several recommendations regarding the role of health professionals, pharmacotherapy, behavioural support and advice-based support for smoking cessation.14
Conclusion
Lung cancer care is undergoing a transformation with a focus on early detection through LDCT screening. GPs will play an essential role in identification of patients with high-risk findings and appropriate referral to a lung cancer multidisciplinary team for further assessment. RMT
COMPETING INTERESTS: Dr Leong is Chair of the Thoracic Society of Australia and New Zealand (TSANZ) Lung Cancer Working Party. Dr Siemienowicz has received consulting fees and payment or honoraria from the Royal Australian and New Zealand College of Radiologists; consulting fees or honoraria from the Australian National Lung Cancer Screening Program (NLCSP); support for attending meetings and/or travel from the TSANZ and Lung Foundation Australia; and is a paid member of the NLCSP groups Data Development Working Group and Expert Advisory Committee. Professor Brims is Deputy Chair of the TSANZ Lung Cancer Working Party.
References
1. Australian Institute of Health and Welfare. Cancer data in Australia. Canberra: AIHW; 2024. Available online at: https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/contents/summary (accessed April 2025).
2. Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365: 395-409.
3. de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med 2020; 382: 503-513.
4. Department of Health and Aged Care. About the National Lung Cancer Screening Program. Canberra: Department of Health and Aged Care; 2025. Available online at: https://www.health.gov.au/our-work/nlcsp/about (accessed April 2025).
5. Department of Health and Aged Care. Information for healthcare providers. Canberra: Department of Health and Aged Care. Available online at: https://ncsr.gov.au/information-for-healthcare-providers.html (accessed April 2025).
6. Heart of Australia. National Lung Cancer Screening Program. Chelmer (QLD): Heart of Australia; 2025. Available online at: https://heartofaustralia.com.au/lung-cancer-screening/ (accessed April 2025).
7. Cancer Council Victoria and Department of Health Victoria. Optimal care pathway for people with lung cancer, 2nd edn. Melbourne: Cancer Council Victoria; 2021. Available online at: https://www.cancer.org.au/assets/pdf/lung-cancer-optimal-cancer-care-pathway (accessed April 2025).
8. Nash J, Stone E, Vinod S, et al. Lung cancer (internet‐based) Delphi (LUCiD): A modified eDelphi consensus process to establish Australasian clinical quality indicators for thoracic cancer. Respirology 2024; 29: 1085-1094.
9. Stone E, Rankin N, Currow D, et al. Optimizing lung cancer MDT data for maximum clinical impact – a scoping literature review. Translational lung cancer research 2020; 9: 1629.
10. Gould MK, Tang T, Liu IL, et al. Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med 2015; 192: 1208-1214.
11. Osarogiagbon RU, Liao W, Faris NR, et al. Lung cancer diagnosed through screening, lung nodule, and neither program: a prospective observational study of the detecting early lung cancer (DELUGE) in the Mississippi Delta Cohort. J Clin Oncol 2022; 40: 2094-2105.
12. Leong TL, McWilliams AM, Wright GM. Incidental pulmonary nodules: an opportunity to complement lung cancer screening. J Thorac Oncol 2024; 19: 522-524.
13. Kauczor HU, Baird AM, Blum TG, et al. ESR/ERS statement paper on lung cancer screening. Eur Radiol 2020; 30: 3277-3294.
14. Royal Australasian College of General Practitioners. Supporting smoking cessation: a guide for health professionals. Melbourne: RACGP; 2024. Available online at: https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/supporting-smoking-cessation (accessed April 2025).