Influenza vaccination in the over 65s — winter is coming

Influenza infection, particularly with influenza A(H3N2) strains, can cause severe morbidity and mortality in older people. Enhanced adjuvanted and high-dose vaccines that provide superior protection than conventional quadrivalent inactivated influenza vaccines are available for people aged 65 years and older. With the possibility of an early influenza season predominated by influenza A(H3N2) in 2023, these enhanced vaccines should be offered to people in this age group. Adjuvanted vaccines are provided free for this age group under the National Immunisation Program.
- In Australia, most cases of serious influenza disease and influenza-related deaths occur in adults aged 65 years and older; long-term sequelae that impact on activities of daily living are also common in this group.
- Standard influenza vaccines offer suboptimal levels of protection in older adults. Two enhanced influenza vaccines are available in Australia for this population; both have a good safety profile.
- The adjuvanted influenza vaccine may provide enhanced protection to older adults and is recommended and funded under the National Immunisation Program (NIP) for people aged 65 years and older in 2023.
- A high-dose version of the standard trivalent vaccine may also provide enhanced protection to older people; however, it is not funded under the NIP in 2023.
- With Omicron variants of the SARS-CoV-2 virus continuing to circulate in Australia, with significant associated mortality, the possibility of combined infections exists this coming winter.
- General practice staff are key partners in encouraging and increasing the level of vaccination coverage in older people.
- This year, the message to get older people vaccinated will require extra effort from immunisers to counter the ‘post- COVID’ vaccine hesitancy in this age group, reflected by poor COVID booster uptake numbers.
Influenza virus infection can cause serious illness resulting in severe burden on the Australian healthcare system. The WHO estimates that, globally, seasonal influenza causes three to five million cases of severe illness and 290,000 to 650,000 deaths every year.1 Influenza affects both industrialised and developing countries. Although data are limited, a recent meta-analysis estimated 82% of deaths in children aged under 5 years with influenza-related acute lower respiratory tract infections occurred in lower-middle income countries.2 However, influenza more often results in severe disease in people with chronic underlying conditions and older people, and most influenza-associated mortality occurs in older adults.3
Influenza in older people
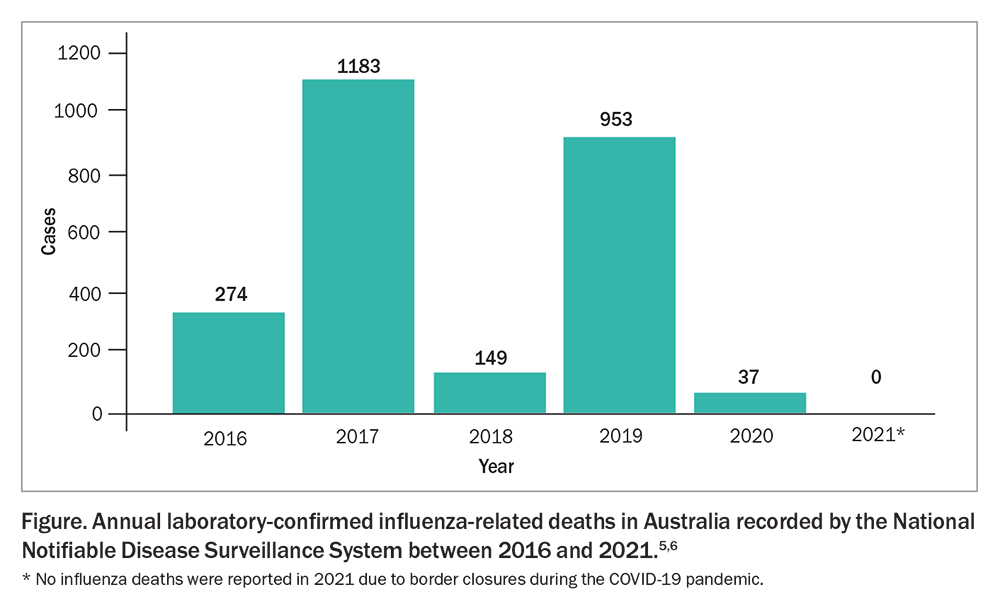
The epidemiology of influenza infections has been chaotic since the arrival of the SARS-CoV-2 virus pandemic. After an intense prolonged influenza season in 2019,4 the nonpharmaceutical interventions in 2020 and 2021 (i.e. lockdown and border closures) led to an absence of influenza in the winter of both those years. After international borders opened and community restrictions were eased, influenza came roaring back with an early peak in April and May of 2022 (Figure).5,6
In 2019, the largest nonpandemic influenza season on record in Australia (313,000 notifications), 86% of the reported 902 influenza-related deaths were in people over 65 years of age.4 Much of the impact of influenza in older people is hidden and presents as previously undetected underlying medical conditions or as a worsening of existing conditions, especially cardiovascular disease.7 For example, acute influenza can lead to decompensation in patients with congestive heart failure or diabetes mellitus and to an increased risk of myocardial infarction and stroke. As patients with these conditions are rarely tested for influenza, the burden of disease is greatly underestimated.8
Influenza can present differently in older adults, who often have a lower incidence of fever; less respiratory symptoms, such as cough, wheezing and chest pain; and atypical disease, with anorexia, mental status changes or unexplained fever as the only presenting symptoms.9,10 Patients with underlying chronic obstructive pulmonary disease may experience worsening respiratory status. Acute myocardial infarctions or heart failure may be unrecognised complications.11,12 Pneumonia is a relatively common complication, especially in people with chronic cardiopulmonary disease.13 Influenza may also significantly impair glucose control in patients with diabetes.14
Older people hospitalised with influenza are more likely to experience a decline in the capacity for activities of daily living after infection.15,16 The occurrence of permanent disabilities from influenza-related illness is increasing as populations age, causing major suffering in older adults and mandating the search for effective prevention programs.17
Influenza virus types
Two influenza virus types predominantly cause human illness: influenza A and influenza B, each with distinct characteristics and effects on different age groups. Influenza A viruses cause more severe illness and are further subdivided into subtypes A(H1N1) and A(H3N2), according to differences in the two surface proteins haemagglutinin (H) and neuraminidase (N). Influenza A has the greatest impact on older adults and young infants, whereas influenza B is more likely to occur in those aged under 20 years.18
The highest rates of influenza-related morbidity and mortality occur in people aged over 65 years infected with A(H3N2) strains.19 There is a direct relationship between seasons when an influenza A(H3N2) strain is the predominant strain in circulation and increased hospitalisations with influenza-associated respiratory and circulatory conditions. No link has been shown between levels of circulation of influenza B viruses and excess mortality or seasonal surges in hospitalisations.20,21
Influenza vaccine responses in older people
An age-related decline in immune function that impairs the ability of older people to fight natural infections is known as immunosenescence and also results in suboptimal immune responses to influenza vaccines.22 Both adaptive and innate immunity decline with age in those aged over 65 years. Influenza vaccine effectiveness in older people varies according to the circulating strain, and is lower in years when influenza A(H3N2) predominates. Older adults have the poorest antibody-mediated immune responses to the A(H3N2) components of vaccines and also display lower cellular immunity to influenza A(H3N2).
Results of previous studies showing that standard influenza vaccination offered little protection in this older age group may have been clouded by a mismatch in some years between viral strains in the vaccine and those circulating in the population, and the different outcomes evaluated. Indeed, studies have shown that vaccination with inactivated influenza vaccine may halve the incidence of laboratory-confirmed and clinical influenza and decrease the severity of disease, as evidenced by lower hospitalisation rates and fewer admissions to intensive care units, in those infected.23,24
The introduction of a new adjuvanted vaccine, initially trivalent but now quadrivalent, has significantly improved vaccine protection in older people. In 2019, data from Queensland showed a 60% reduction in hospitalisations in those aged over 65 years after the introduction of the quadrivalent adjuvanted vaccine, compared with a similarly intense year in 2017, when nonadjuvanted vaccine was used to vaccinate this group.25,26 Vaccine effectiveness data from 2019 revealed that nonadjuvanted vaccine was more effective in older people compared with younger people using traditional quadrivalent inactivated vaccines, despite immunosenescence issues.27
Influenza vaccines recommended for older people
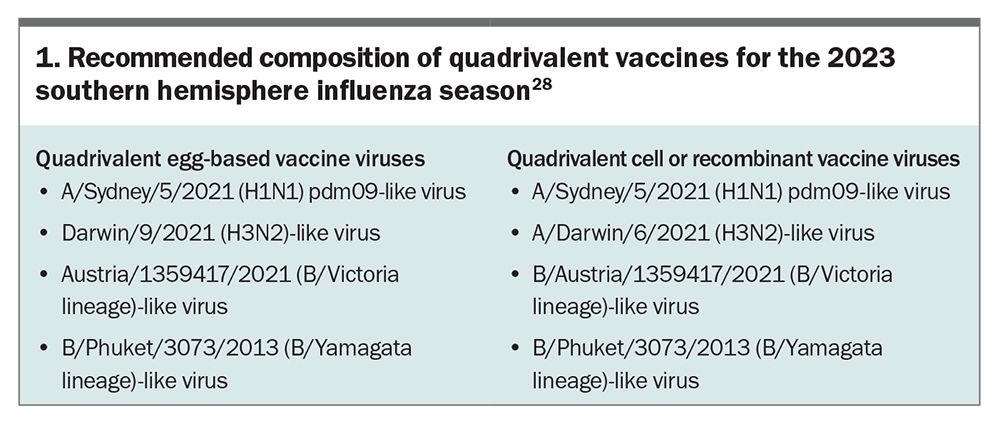
Influenza vaccination is recommended and funded in Australia for all people aged 65 years and older. The most widely used influenza vaccines are quadrivalent formulations of inactivated haemagglutinin and neuraminidase antigens, representative of the predominant A(H1N1), A(H3N2) and both B lineages, using the selected strains for each season recommended by the Australian Influenza Vaccination Committee. The recommended strains for the influenza vaccines for the 2023 southern hemisphere influenza season are listed in Box 1.28
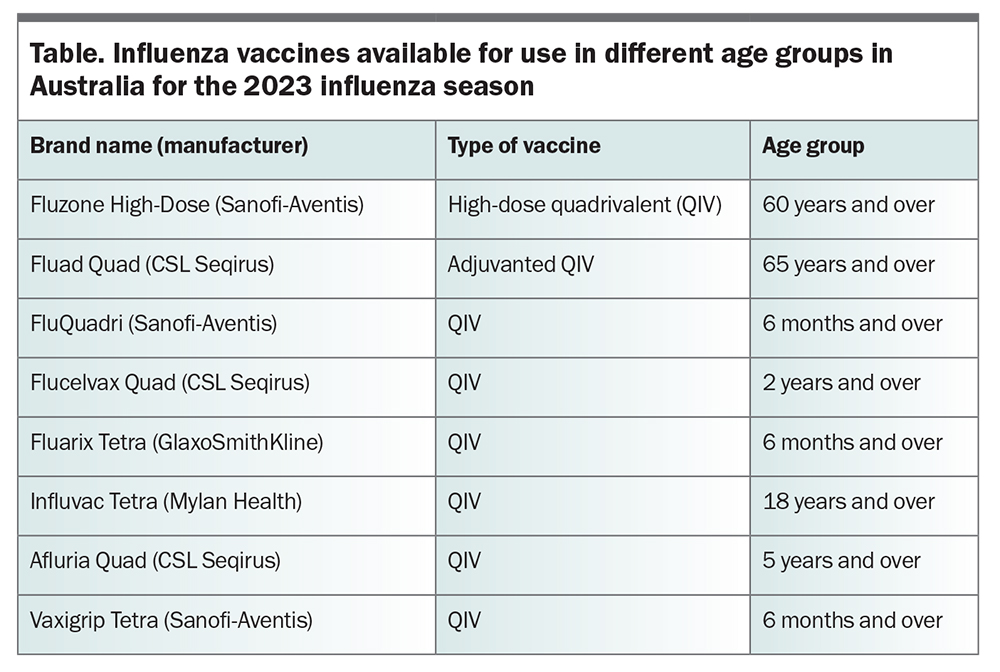
Enhanced vaccines are required to provide adequate protection in older people.22 The Australian Government funded two new enhanced vaccines for people aged 65 years and over for the first time in 2018: an adjuvanted vaccine and a high-dose vaccine. Both vaccines showed improved effectiveness in real-world studies and elicited greater antibody responses than standard influenza vaccines in clinical trials. Vaccines available in Australia in 2023 are shown in the Table.
Since 2019, only the adjuvanted vaccine has been provided at no cost under the National Immunisation Program (NIP), although the high-dose vaccine is available on the private market and is now licensed for the 60 to 64 years age group as well as those 65 years and over.
Enhanced influenza vaccines
Adjuvanted influenza vaccine
The adjuvanted influenza vaccine both enhances the magnitude of and broadens the immune response to improve protection during years when vaccine strains do not match circulating viruses.29,30 The adjuvant MF59 is an oil-in-water emulsion based on squalene, which enhances both antigen presentation and T-cell priming. Importantly, a number of international studies of adjuvanted influenza vaccine found a significant increase in the response to influenza A(H3N2) in people aged over 65 years.31,32 In 2023, the adjuvanted influenza vaccine is recommended as one of the two preferred vaccines for use in older people and is the only one funded under the NIP.
High-dose influenza vaccine
The high-dose influenza vaccine contains 60 mcg haemagglutinin per strain, instead of 15 mcg, and produces a dose-dependent increase in antibody response. It has been shown to induce a higher immune response in older adults, with improved efficacy against influenza infection compared with the standard influenza vaccine in clinical trials.33,34 Although the high-dose influenza vaccine is recommended as one of the two preferred vaccines for use in older people, it is not funded under the NIP.
Benefit of enhanced vaccines
The predominant circulating strain (A(H3N2) or other) and the degree of match with the vaccine strains determine the attributable additional benefit of using an enhanced vaccine (adjuvanted or high dose) in any given year. However, several real-world studies on the effectiveness of enhanced vaccines in older people have shown about 25% extra protection against disease, and even higher additional protection against severe disease.32 This additional protection has enormous implications for improving the burden of disease associated with influenza in older people and research is currently underway to quantify these benefits in Australia.
Safety of enhanced vaccines
The adjuvanted trivalent influenza vaccine has established a good safety record since it was licensed 20 years ago, with an analysis of 20,000 vaccinations showing a higher risk of solicited local or systemic reactions, but no increase in severe adverse effects or longer-term consequences.35 High-dose trivalent influenza vaccines showed a similar small increase in local injection site reactions, most commonly pain at the site, and some increase in the rate of systemic adverse events. These reactions were largely mild and self-limiting, with no increase in the rate of serious adverse events.36
Timing of influenza vaccination in older people
Data on influenza vaccine effectiveness over the course of the influenza season suggest that in a predominant A(H3N2) season, vaccine effectiveness falls about 8% per month, and vaccines may be ineffective four months after administration. In the years before COVID-19, influenza infections predominated in June, with vaccinations administered in May. However, given the influenza season occurred earlier in 2022, mainly during April and May, and may do so again this year, delaying vaccination until May no longer appears warranted, and vaccine should be used as soon as available. Immunological markers have been shown to persist for more than six months after administration of adjuvanted influenza vaccine; therefore, timing of vaccination may be less crucial with this vaccine.
Influenza in the era of COVID-19
Although the emphasis on SARS-CoV-2 circulation in Australia has largely disappeared from both media and political commentary, regular waves of COVID-19 Omicron variants continue. At the end of January 2023, Victoria alone saw an average of 50 deaths a day from SARS-CoV-2 infection and over 800 aged care facilities experienced COVID-19 outbreaks. In the first two months of 2023, 2409 people died from COVID-19, more than the numbers in both 2020 and 2021. The ongoing morbidity and mortality, in older people in particular, are associated with a decrease in the uptake of COVID-19 vaccine boosters in people of all ages.
This vaccine hesitancy may roll over to influenza vaccine uptake this year with potentially severe consequences. Outbreaks of influenza A(H3N2) already occurring in neighbouring Asian countries suggest that it will likely be the dominating subtype this winter in Australia, and have greatest impact on older people. The likelihood that both influenza and SARS-CoV-2 will circulate together this winter is high. NIP-funded influenza vaccines for those aged 65 years and older are available now and vaccination should be encouraged as soon as possible in this age group.
Role of GPs
Vaccination is an important component of promoting healthy ageing. The coverage rate for influenza vaccination in people aged 65 years and older was 68.9% at the end of August 2022.37 Although this was the highest rate of any age group, given its clear benefits in this age group, influenza vaccination for older people should continue to be encouraged, with the aim of increasing coverage rates.
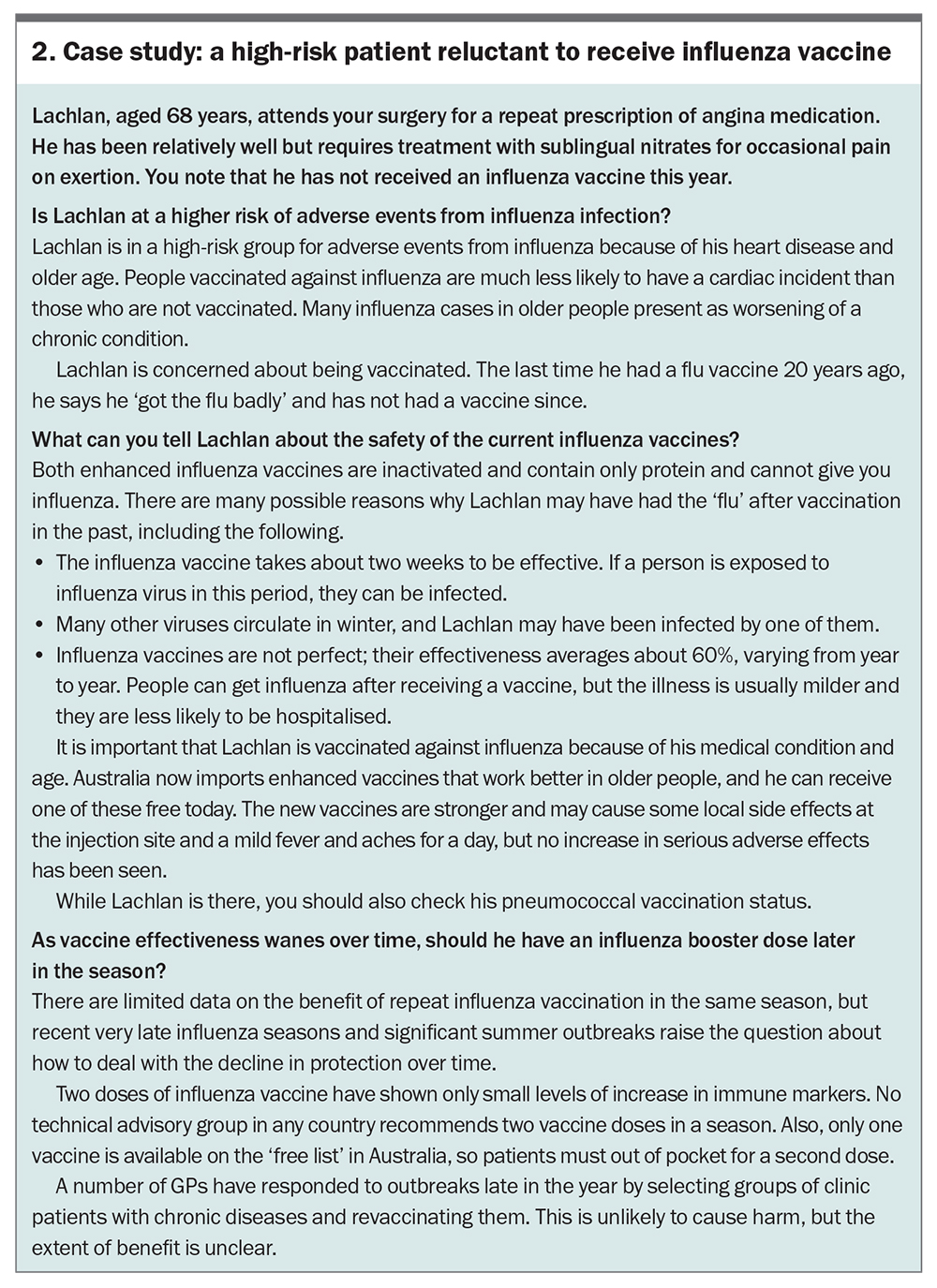
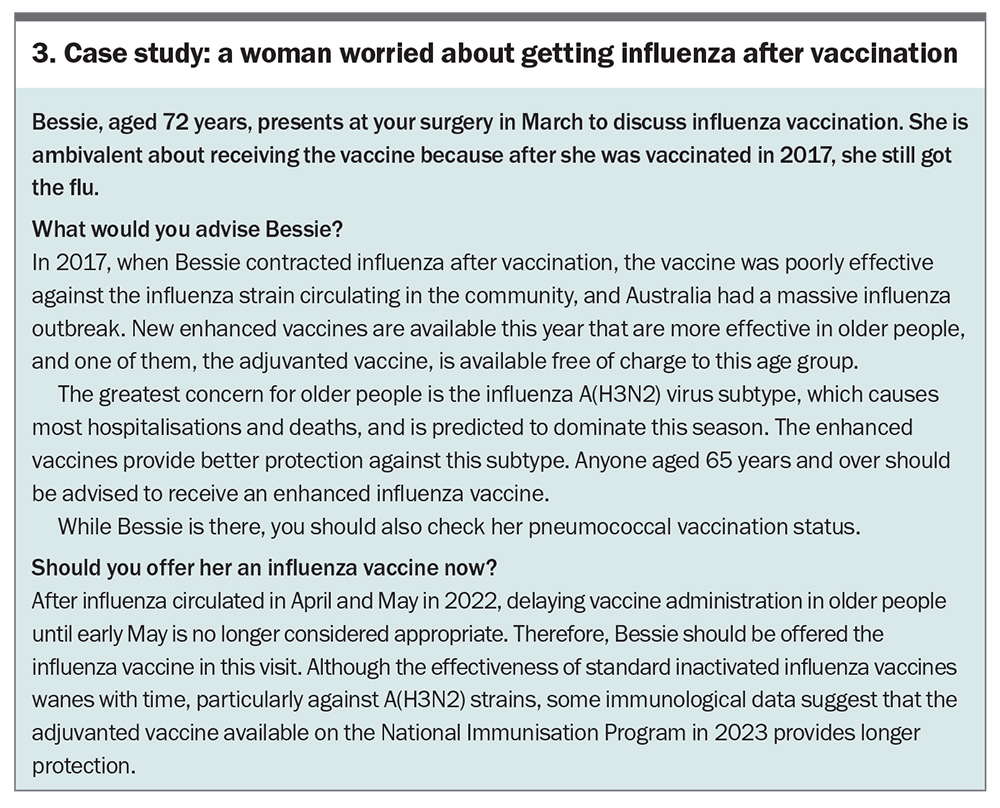
GPs are key to improving vaccination rates.38 Clearly communicating the rationale for vaccination in older people, including the high risk of morbidity and mortality with influenza virus infection and the benefit of vaccination with a new, safe enhanced vaccine, with all patients in target groups is important, particularly those with chronic disease. Two case studies illustrating this approach are shown in Box 2 and Box 3.
Conclusion
Influenza remains a major public health problem in Australia that causes significant severe disease, long-term disability and mortality in older people. The theoretical advantages of adding an adjuvant have translated to real-world studies to improved protection for older people. For this reason, the use of an adjuvanted influenza vaccine in people aged 65 years and older is recommended and funded under the NIP for this age group. Healthcare practitioners should note these recommendations and ensure that their older patients are offered this seasonal vaccine designed specifically to protect older people. RMT
COMPETING INTERESTS: Professor Van Buynder has conducted clinical research on vaccine effectiveness of adjuvanted vaccines via an unrestricted grant from Novartis. He has also received support for research, education and marketing, travel and/or advisory board activities from Seqirus, Sanofi, GlaxoSmithKline, Roche, Pfizer Merck and Novartis.
References
1. World Health Organization. Fact sheet. Influenza (seasonal). Geneva: WHO; 2023. Available online at: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal) (accessed March 2023).
2. Wang X, Li Y, O’Brien KL, et al; Respiratory Virus Global Epidemiology Network. Global burden of respiratory infections associated with seasonal influenza in children under 5 years in 2018: a systematic review and modelling study. Lancet Glob Health 2020; 8(4): e497-e510.
3. US Centers for Disease Control and Prevention. Disease burden of influenza. Atlanta, GA: CDC;2019. Available online at: www.cdc.gov/flu/about/ disease/burden.htm (accessed March 2023).
4. Department of Health. 2019 Influenza Season in Australia. A summary from the National Influenza Surveillance Committee. Canberra; Department of health, 2021. Available online at: https://www.health.gov.au/sites/default/files/documents/2022/10/aisr-2019-national-influenza-season-summary.pdf (accessed March 2023).
5. Department of Health. National 2020 influenza season summary. Canberra; Department of health, 2020. Available online at: https://www.health.gov.au/sites/default/files/documents/2022/10/aisr-2020-national-influenza-season-summary.pdf (accessed March 2023).
6. Hood J, ed. Report of the National Influenza Surveillance Scheme, 2011 to 2018. Communicable Diseases Intelligence 2022; 46. Canberra; Department of health, 2022. Available online at: https://www1.health.gov.au/internet/main/publishing.nsf/Content/8FA6078276359430CA257BF0001A4C42/$File/
report_of_the_national_influenza_surveillance_scheme_2011_to_2018.pdf (accessed March 2023).
7. Siriwardena AN. Increasing evidence that influenza is a trigger for cardiovascular disease. J Infect Dis 2012; 206: 1636-1638.
8. Gordon A, Reingold A. The burden of influenza: a complex problem. Curr Epidemiol Rep 2018; 5: 1-9.
9. Falsey AR, Baran A, Walsh EE. Should clinical case definitions of influenza in hospitalized older adults include fever? Influenza Other Respir Viruses 2015; 9 Suppl 1: 23-29.
10. Minnesota Department of Health (US). Influenza-like illness in elderly persons. St Paul, MN: Department of Health; 2016. Available online at: www.health.state.mn.us/diseases/flu/ltc/fluelderly.html (accessed March 2023).
11. Caldeira D, Rodrigues B, David C, Costa J, Pinto FJ, Ferreira JJ. The association of influenza infection and vaccine with myocardial infarction: systematic review and meta-analysis of self-controlled case series. Expert Rev Vaccines 2019; 18: 1211-1217.
12. Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med 2018: 378: 345-53.
13. Zhou H, Thompson WW, Viboud CG, et al. Hospitalisations associated with influenza and respiratory syncytial virus in the United States 1993-2008. Clin Infect Dis 2012; 54: 1427-1436.
14. Hulme KD, Gallo LA, Short KR. Influenza virus and glycemic variability in diabetes: a killer combination? Front Microbiol 2017; 8: 861.
15. Gozalo PL. The impact of influenza on functional decline. J Am Geriatr Soc 2012; 60: 1260-1267.
16. Haq K, McElhaney JE. Immunosenescence: influenza vaccination and the elderly. Curr Opin Immunol 2014; 29: 38-42.
17. Keilich SR, Bartley JM, Haynes L. Diminished immune responses with aging predispose older adults to common and uncommon influenza complications. Cellular immunity 2019; 345: 103992.
18. US Centers for Disease Control and Prevention. Types of influenza viruses. Atlanta, GA: CDC; 2017. Available online at: www.cdc.gov/flu/about/viruses/types.htm (accessed March 2023).
19. Czaja CA, Miller L, Alden N, et al. Age-related differences in hospitalization rates, clinical presentation, and outcomes among older adults hospitalized with influenza—U.S. Influenza Hospitalization Surveillance Network (FluSurv-NET). Open Forum Infect Dis 2019; 6: ofz225.
20. Cromer D, van Hoek AJ, Jit M, Edmunds WJ, Fleming D, Miller E. The burden of influenza in England by age and clinical risk group: a statistical analysis to inform vaccine policy. J Infect 2014; 68: 363-371.
21. Schanzer DL, Sevenhuysen C, Winchester B, Mersereau T. Estimating influenza deaths in Canada 1992-2009. PLoS One 2013; 8: e80481.
22. McElhaney JE, zhou X, Talbot HK, et al. The unmet need in the elderly: how immunosenescence, CMV infection, co-morbidities and frailty are a challenge for the development of more effective influenza vaccines. Vaccine 2012; 30: 2060-2067.
23. Govaert TM, Thijs CT, Masurel N, Sprengel MJ, Dinant GJ, Knotterus JA. The efficacy of influenza vaccination in elderly individuals. A randomised double-blind placebo-controlled trial. JAMA 1994; 272: 1661-1665.
24. Godoy P, Romero A, Soldevilla N, et al; The Working Group on Surveillance of Severe Influenza Hospitalized Cases in Catalonia. Influenza vaccine in reducing severe outcomes over six influenza seasons, a case-case analysis, Spain, 2010-11 to 2015-16. Euro Surveill 2018; 23: 1700732.
25. Queensland Health. Statewide Weekly Influenza Surveillance Report. Queensland; Queensland Health, 2018. Available online at: https://www.health.qld.gov.au/__data/assets/pdf_file/0034/656494/influenza-qld-2017.pdf (accessed March 2023).
26. Queensland Health. Statewide Weekly Influenza Surveillance Report. Queensland; Queensland Health, 2019. Available online at: https://www.health.qld.gov.au/__data/assets/pdf_file/0037/835588/influenza-qld-2019.pdf (accessed March 2023).
27. Sullivan S, Arriola C, Bocacao J, et al. Heterogeneity in influenza seasonality and vaccine effectiveness in Australia, Chile, New Zealand and South Africa: early estimates of the 2019 influenza season Euro Surveill 2019; 24: 1900645.
28. WHO. New recommendations for the composition of influenza vaccines in 2023 for the southern hemisphere. Geneva; WHO, September 2022. Available online at: https://www.who.int/news/item/23-09-2022-new-recommendations-for-the-composition-of-influenza-vaccines-in-2023-for-the-southern-hemisphere (accessed March 2022).
29. Frey SE, Reyes MR, Reynales H, et al. Comparison of the safety and immunogenicity of an MF59®-adjuvanted with a non-adjuvanted seasonal influenza vaccine in elderly subjects Vaccine. 2014; 32: 5027-5034.
30. Nicolay U, Heijnen E, Nacci P, Patriarca PA, Leav B. Immunogenicity of aIIV3, MF59-adjuvanted seasonal trivalent influenza vaccine, in older adults ≥65 years of age: meta-analysis of cumulative clinical experience. Int J Infect Dis 2019; 85S: S1-S9.
31. Van Buynder PG, Konrad S, Van Buynder JL, et al. The comparative effectiveness of adjuvanted and unadjuvanted trivalent inactivated influenza vaccine (TIV) in the elderly. Vaccine 2013; 31: 6122-6128.
32. Domnich A, Arata L, Amicizia D, Puig-Barbera J, Gasparini R, Panatto D. Effectiveness of MF59-adjuvanted seasonal influenza vaccine in the elderly: a systematic review and meta-analysis. Vaccine 2017; 35: 513-520.
33. DiazGranados CA, Dunning AJ, Kimmel M, et al. Efficacy of high-dose versus standard dose influenza vaccine in older adults. N Engl J Med 2014; 371: 635-645.
34. Wilkinson K, Wei Y, Szwajcer A, et al. Efficacy and safety of high-dose influenza vaccine in elderly adults: a systematic review and meta-analysis. Vaccine 2017; 35: 2775-2780.
35. Pellegrini M, Nicolay U, Lindert K, Groth N, Della Cioppa G. MF59- adjuvanted versus non-adjuvanted influenza vaccines: integrated analysis from a large safety database. Vaccine 2009; 27: 6959-6965.
36. Couch RB, Winokur P, Brady R, et al. Safety and immunogenicity of a high dosage trivalent influenza vaccine among elderly subjects. Vaccine 2007; 25: 7656-7663.
37. National Centre for Immunisation Research and Surveillance (NCIRS). Influenza vaccination coverage data. Sydney; NCIRS; 2022. Available online at: https://ncirs.org.au/influenza-vaccination-coverage-data (accessed March 2023).
38. Litt J, Rigby K, Duffy J. Australian National Influenza and Pneumococcal Survey in the elderly. Report No. 1. 12/2003 to Commonwealth Department of Health and Ageing. Adelaide: Discipline of General Practice, Flinders University; 2003.