Pulmonary rehabilitation: a breath of fresh air for patients with chronic respiratory disease

Pulmonary rehabilitation reduces symptoms, increases exercise capacity and decreases hospital admissions for people with chronic respiratory disease. New models of pulmonary rehabilitation are becoming available, including home-based programs and telerehabilitation, which may increase the accessibility and uptake of this important treatment.
- Pulmonary rehabilitation is a program of exercise, education and self-management training for people with chronic respiratory disease.
- Pulmonary rehabilitation improves symptoms and health-related quality of life and reduces hospital admissions in people with chronic respiratory disease.
- The inclusion criteria for pulmonary rehabilitation are broad, and most patients with chronic respiratory disease are eligible to attend.
- A referral to pulmonary rehabilitation can be made by any healthcare professional.
- New models of pulmonary rehabilitation, including telerehabilitation, may improve access to this important treatment.
Chronic respiratory diseases, including chronic obstructive pulmonary disease (COPD), bronchiectasis and interstitial lung disease, accounted for 7.3% of Australia’s total disease burden in 2022.1 The disease burden related to COPD increased between 2003 and 2022, in part reflecting the ageing population. From 2017 to 2018, COPD accounted for more potentially preventable hospitalisations than any other chronic condition.2 People with chronic respiratory disease often experience breathlessness, cough, fatigue and reduced exercise capacity. Although chronic respiratory diseases in adults are often not reversible, a range of pharmacological and nonpharmacological treatments can effectively reduce symptoms, enhance wellbeing and reduce hospital admissions. Pulmonary rehabilitation is a crucial but underutilised part of this treatment package. This article provides an overview of the practicalities of pulmonary rehabilitation and how the treatment can be implemented to benefit patients with chronic respiratory disease.
What is pulmonary rehabilitation?
Pulmonary rehabilitation is a comprehensive intervention involving a thorough patient assessment and patient-tailored therapies, including, but not limited to, exercise training, education and behaviour change. The intervention aims to improve the physical and psychological condition of people with chronic respiratory disease and to promote long-term adherence to health-enhancing behaviours.3 Pulmonary rehabilitation programs usually last for eight to 12 weeks, with two supervised group sessions each week lasting approximately one hour, delivered in an outpatient setting, such as a hospital or community health centre.4
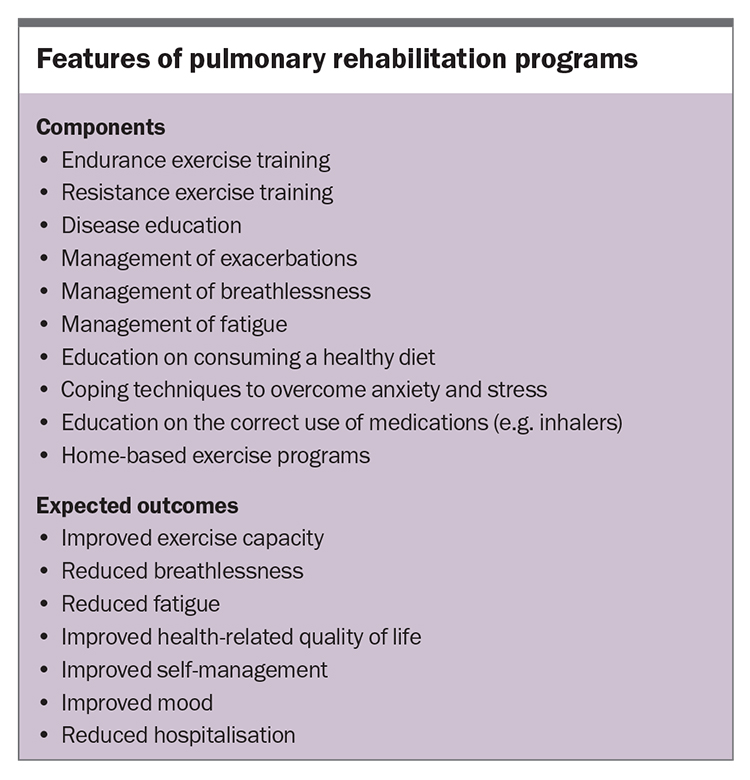
Typical features of pulmonary rehabilitation programs are outlined in the Box. Exercise training is a core component of these programs. The exercise prescription is specifically tailored for individuals with chronic respiratory disease and is typically supervised by a physiotherapist or exercise physiologist. Other components may include information sessions on the correct use of medications (including inhalers); the management of breathlessness, fatigue and exacerbations of lung disease; and education on how to remain fit after pulmonary rehabilitation. A typical pulmonary rehabilitation session comprises supervised exercise training (endurance exercises, such as walking or stationary cycling, plus resistance exercises, such as the use of light dumbbells, body weights or resistance machines), as well as individualised education and self-management training delivered by members of the multidisciplinary team.
Expected outcomes of pulmonary rehabilitation
Evidence from clinical trials shows that pulmonary rehabilitation reduces breathlessness and fatigue, improves exercise capacity and enhances health-related quality of life across numerous chronic respiratory diseases, including COPD, asthma, bronchiectasis and interstitial lung disease.5-7 In patients with COPD, there is also convincing evidence that pulmonary rehabilitation delivered after hospitalisation for an exacerbation reduces mortality and hospital readmissions.8 Other benefits of pulmonary rehabilitation reported by participants include improved physical functioning in daily life, improved mood, greater knowledge about their pulmonary condition, better control of symptoms and enhanced social functioning.9 The strong evidence supporting the benefits of pulmonary rehabilitation has led to recommendations for its delivery in Australian and international clinical guidelines.10-12
Who is eligible for pulmonary rehabilitation?
The eligibility criteria for pulmonary rehabilitation are broad, and few patients are excluded. Patients are eligible for pulmonary rehabilitation if they:
- have a diagnosis of chronic respiratory disease, including COPD, bronchiectasis, interstitial lung disease, chronic asthma, lung cancer or pulmonary hypertension
- are in a stable clinical state or are recovering from an acute exacerbation of their condition
- are willing to participate (even if they are on long-term oxygen therapy or are current smokers)
- are at any stage of their disease.
Comorbidities, such as cardiovascular disease and osteoarthritis, do not exclude patients from participating in pulmonary rehabilitation. Before starting the program, all patients undergo a thorough assessment, including evaluations of symptoms, limitations to daily activities and disease management skills, as well as an exercise test to ensure it is safe for them to exercise. In most cases, the exercise program can be individually tailored to account for comorbid conditions. Many pulmonary rehabilitation programs will accept patients with persistent symptoms or functional impairment following COVID-19, including those with long COVID.
How to refer patients to pulmonary rehabilitation
There are more than 300 pulmonary rehabilitation programs in Australia. These can be found at most healthcare services in metropolitan areas and large regional centres, as well as some private hospitals. A full list of pulmonary rehabilitation exercise classes (which include education sessions) available in Australia and the relevant contact details can be found on the Lung Foundation Australia’s website (https://lungfoundation.com.au/patients-carers/support-services/lung-disease-and-exercise/exercise-classes/). Some programs may have referral templates available on the local HealthPathways website.
General practitioners, respiratory specialists, general physicians, thoracic surgeons, oncologists and other allied healthcare professionals can refer eligible patients to pulmonary rehabilitation. Patients can also self-refer to some of these programs. Many patients are not aware of the option of pulmonary rehabilitation, and primary care visits may provide an opportunity to engage in a discussion with patients about the potential benefits of such programs and offer a referral.
Useful information to include in a referral includes the patient’s respiratory diagnosis, history of exacerbations and hospitalisations, other medical conditions, relevant investigations (e.g. lung function test results) and medications, any special requirements for attendance (e.g. transport requirements) and contact details.
Patients with chronic respiratory disease may be nervous about attending a pulmonary rehabilitation program, as their experience of breathlessness often results in the avoidance of exercise. When discussing a referral with a patient, it is helpful to describe the components of the program and provide reassurance that the program will be individually tailored to their symptoms and needs. The enthusiasm of the referring doctor is a key facilitator of pulmonary rehabilitation uptake.13
Following referral to a program, the patient will be contacted by the program co-ordinator and sent an invitation to participate, detailing the assessment appointment, days and times for the program, and parking and transport options for the facility.
Improving access to pulmonary rehabilitation: home-based and telerehabilitation models
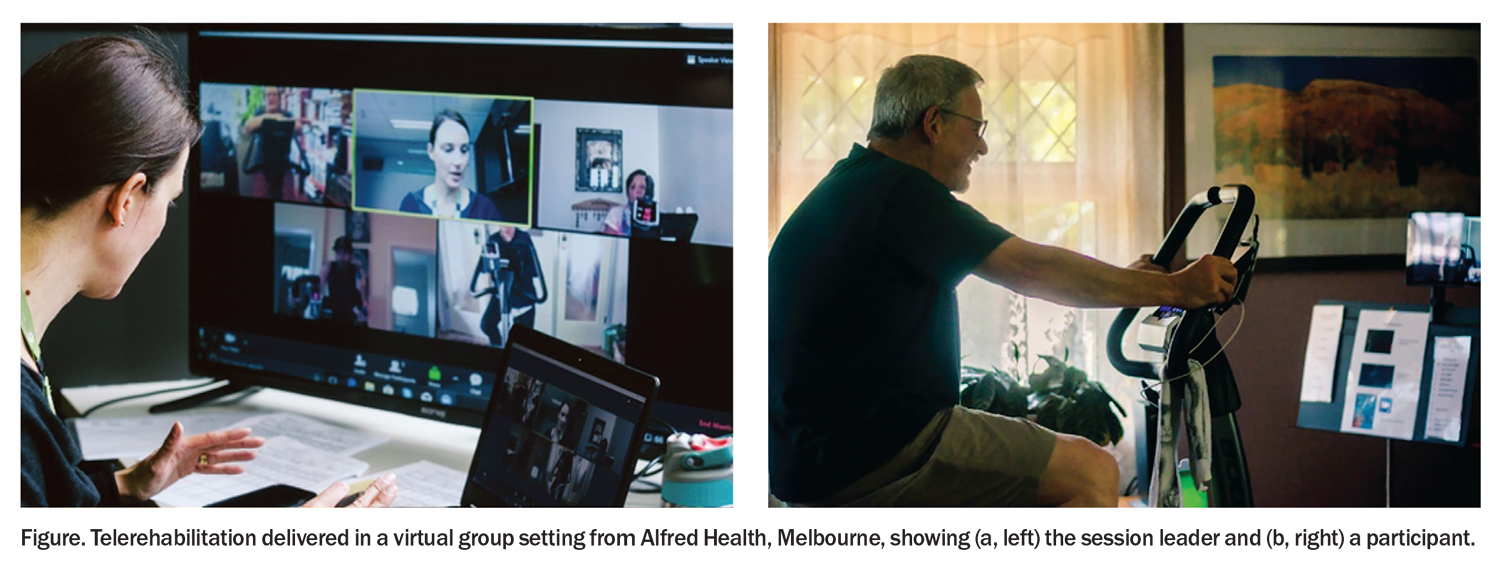
In recent years, new models of pulmonary rehabilitation have emerged that can be delivered directly to the home, which overcomes access barriers. Telerehabilitation aims to deliver rehabilitation services from a distance using information and communication technology.14 Pulmonary rehabilitation delivered via telerehabilitation may include the use of a telephone, the Internet or videoconferencing. Telephone models are simple and suitable for patients with limited access to technology, but they do not allow for direct supervision of exercise training and often rely on physical activity coaching to achieve improvements in physical capacity. Internet models offer patients the flexibility of working through the program at their own pace, but they may have minimal interaction with healthcare professionals or other patients. More technologically complex models may use videoconferencing to allow for direct supervision of home-based exercise training in real time, often in a virtual group setting, which also allows patients to experience the benefits of peer support (Figure).
Telerehabilitation achieves outcomes similar to those of traditional centre-based pulmonary rehabilitation, in terms of exercise capacity and health-related quality of life for patients with chronic respiratory disease, and has higher completion rates.14 The COVID-19 pandemic has accelerated the adoption of telerehabilitation by Australian pulmonary rehabilitation programs; however, it is not yet offered at all centres. Although telerehabilitation improves access for patients who would not otherwise be able to participate in pulmonary rehabilitation, it is not for everyone. Important considerations when considering telerehabilitation include the patient’s access to technology; digital literacy; communication abilities, including language, hearing and sight; cognition; safety of the home environment; falls risk while exercising at home; and patient preference for a home- or centre-based model.
Conclusion
Pulmonary rehabilitation improves symptoms, exercise capacity and health-related quality of life for patients with a range of respiratory diseases. It also plays a key role in reducing hospital admissions for COPD exacerbations. Emerging telerehabilitation models provide opportunities to increase the uptake of this important treatment. RMT
COMPETING INTERESTS: Ms Mellerick: None. Professor Holland is on the Board of Directors at the Thoracic Society of Australia & New Zealand.
References
1. Australian Institute of Health and Welfare (AIHW). Australian Burden of Disease Study 2022. Canberra: AIHW, Australian Government; 2022. Available online at: https://www.aihw.gov.au/getmedia/d9ae4bfa-df27-4e3c-9846-ba452bef6ac5/aihw-bod-37.pdf.aspx?inline=true (accessed March 2023).
2. Australian Institute of Health and Welfare (AIHW). Disparities in potentially preventable hospitalisations across Australia, 2012-13 to 2017-18. Canberra: AIHW, Australian Government; 2020. Available online at: https://www.aihw.gov.au/getmedia/20bc5bf9-d46c-40a7-96c1-d632a1d448bc/aihw-hpf-50.pdf.aspx?inline=true (accessed March 2023).
3. Holland AE, Cox NS, Houchen-Wolloff L, et al. Defining modern pulmonary rehabilitation. An official American Thoracic Society workshop report. Ann Am Thorac Soc 2021; 18: e12-e29.
4. Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013; 188: e13-e64.
5. Dowman L, Hill CJ, May A, Holland AE. Pulmonary rehabilitation for interstitial lung disease. Cochrane Database Syst Rev 2021; 2: CD006322.
6. Lee AL, Gordon CS, Osadnik CR. Exercise training for bronchiectasis. Cochrane Database Syst Rev 2021; 4: CD013110.
7. McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2015; 2: CD003793.
8. Puhan MA, Gimeno-Santos E, Cates CJ, Troosters T. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2016; 12: CD005305.
9. Rochester CL, Vogiatzis I, Powell P, Masefield S, Spruit MA. Patients’ perspective on pulmonary rehabilitation: experiences of European and American individuals with chronic respiratory diseases. ERJ Open Res 2018; 4: 00085-2018.
10. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of COPD: 2023 report. GOLD; 2023. Available online at: https://goldcopd.org/2023-gold-report-2/ (accessed March 2023).
11. Dabscheck E, George J, Hermann K, et al. COPD-X Australian guidelines for the diagnosis and management of chronic obstructive pulmonary disease: 2022 update. Med J Aust 2022; 217: 415-423.
12. Alison JA, McKeough ZJ, Johnston K, et al. Australian and New Zealand pulmonary rehabilitation guidelines. Respirology 2017; 22: 800-819.
13. Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis 2011; 8: 89-99.
14. Cox NS, Dal Corso S, Hansen H, et al. Telerehabilitation for chronic respiratory disease. Cochrane Database Syst Rev 2021; 1: CD013040.